More Information
Submitted: 19 August 2019 | Approved: 02 September 2019 | Published: 02 September 2019
How to cite this article: Ngaithianven E, Sehrawat JS, Kaur R. Does it matter what a mother consumes? An anthropological exploration of dietary practices among Churachandpur (Manipur) pregnant women and its impact on infant birth weight. J Adv Pediatr Child Health. 2019; 2: 008-014.
DOI: 10.29328/journal.japch.1001005
Copyright License: © 2019 Sehrawat JS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Food taboos; Mean baby weight; Paite; Pica; Taboo; India
Does it matter what a mother consumes? An anthropological exploration of dietary practices among Churachandpur (Manipur) pregnant women and its impact on infant birth weight
Evelyn Ngaithianven, JS Sehrawat* and Reetinder Kaur
Department of Anthropology, Panjab University, Chandigarh, India
*Address for Correspondence: Jagmahender Singh Sehrawat, Assistant Professor, Department of Anthropology, Panjab University, Chandigarh, India, Email: [email protected]; [email protected]
Background: Nutritional status of expectant women is an important indicator of healthy pregnancy and an ideal birth weight of the infant. The present study is an attempt to understand food eating practices and related taboos among the Paite women and whether or how these practices influence weight gain among infants during their first year of life.
Methods: The longitudinal study was conducted for a period of 16 months between November 2010 and February 2012) among 186 Paite mother-infant pairs. Women who had completed 37 to 42 weeks of pregnancy were included. Infant’s weights were measured using standard technique and information on mothers’ food related practices was recorded during the house visit using a structured schedule. Standard statistical methods were used for description and analysis.
Results: A peculiar practice, ‘pica’ was observed among a few women. A number of food taboos were found to be followed by the ‘Paite’ women during course of their pregnancy.
Conclusion: No significant difference was noticed in the mean weight of babies from birth through the age of 1 year between mothers practicing and not practicing food taboos. However, it was found that the mean weight of the babies throughout the study period was comparatively higher among non-taboo mothers. It could be suggested that women must be counseled during their antenatal and postnatal visits to the maternity clinics and hospitals about dietary practices and their anticipated impact on health of the newborns.
Maternal nutritional status during pregnancy is an important indicator of healthy pregnancy and ideal birth weight of the infant [1-6]. Dietary practices during pregnancy, directly or indirectly affects the nutritional status and plays an important role in the overall wellbeing of both mother and the child. These practices are largely governed by cultural norms, taboos and beliefs passed on from generation to generation within a community. The cultural knowledge may affect types of food consumed and avoided, and the quantity of food taken by the mothers as well as the infants. Likewise, the food taboos represent unwritten social rules mainly based on religious and/or historical reasons that regulate food consumption in a community [7]. A significant body of research suggests that pregnant women in various parts of the world are forced to abstain from nutritious foods as a part of their traditional food habits and food taboos [8-10]. According to the UNICEF Food-Care Health conceptual framework, cultural norms, taboos and beliefs lie within the contextual factors included as one of the basic causes of malnutrition [11]. Among the community under study, Paite, the food consumption practice called pica is studied. The word is derived from Latin word for magpie, a bird known for its unusual and indiscriminate eating habits [12]. Pica generally refers to compulsive intake of non-food substances over a sustained period of time [13], which can be in the form of clay, ashes, chalk, burnt matches, charcoal, etc. Although pica had been widely studied in the general population, little was known about its impact on the mother and foetus. Horner et al. [13] noticed the high prevalence of pica in some ethnic groups and called for further study on the conditions among pregnant women to determine any relationships to high infant mortality rates. Further, no study is conducted among the tribal population of Manipur on the prevalence of Pica during pregnancy and this is an attempt to bring to light the prevalence of pica practice among the Paite tribe. The distinction between hot and cold foods is also highlighted. To throw a better light on the food habits of the Paite, some of their staple diets are briefly discussed.
What a woman consumes during pregnancy affects the health of the child. Weight at the time of birth and gained during first year of life is an important predictor for the health of a child. It is an indicator of a new-born’s chances for survival, growth, long-term health and psychosocial development [14]. The birth weight is the result of interplay of factors such as intrauterine growth as well as the nutritional conditions and gestational age at birth. However, eventual weight gain is affected by social and cultural factors such as feeding practices, mothers’ nutritional status, and maintenance of hygiene. Since, infant growth is most rapid during the first year of life, any form of growth deformities can have both short and long term repercussions, including later overweight, which is more common in children with birth weight less than 2500 grams [15]. Similarly, it is noted that low birth weight babies can have difficulties to achieve the NCHS standard weight at 12 months [16]; including greater susceptibility to infections [17] and attenuated cognitive development [18]. Any form of growth deformities can also lead to reduced height [19], reduced capacity to work [20] and increased risk of obesity [21] in adulthood. The importance of linear growth during early childhood and its repercussions throughout life mean that there is a need for more precise estimates of normal growth patterns in this phase of life, based on the results of studies that include means to control for intra-child and inter-child variability. Furthermore, maternal weights during pregnancy are considered good predictors for birth weight by some previous researchers [2,5,22,23]. A number of studies detected a strong relationship between birth weight and nutritional status of mothers as measured using anthropometric techniques [1-3,22,24]. However, establishment of association between maternal anthropometric variables and infant growth patterns through longitudinal research is limited.
Study sites
As per Census of India, 2011, Churachandpur has a population of 2,74,143 people with a literacy rate of 82.7 % and tribal population at 92.9%. The district has an area of 4,570 square kilometer and it is the biggest districts in Manipur covering 20.47 percent of the total geographical area of the state. It has a total of 596 villages in the district. Churachandpur district is currently receiving funds from the Backward Regions Grant Fund Programme (BRGF) and it (the study area) has one government hospital and four registered private maternity hospitals. According to District Health Action Plan for 2013-2014, only 5% of newborn were found weighing less than 2.5 kg and 9.6 still births against reported 1000 live births. It was further reported that 93% of newborn were breastfed within one hour of birth. Even though the central government made many schemes available for pregnant women through Accredited Social Health Activist (National Rural Health Mission), only a handful of mothers were found benefitting. However, with the implementation of National Rural Employment Guarantee Act in the district in 2005, every household had the advantage of employment prospects. Majority of its residents in the district Churachandpur are of Paite ethnicity and Christianity is the religion practiced. Paite is a name of a tribe formed by congeries of clans. Official use of the term came into existence in India since the specification of the term under the provision of Article 342 of the Constitution of India in the modification order of the Constitution, 1956. They are Tibeto-Burmese in speech and Mongoloid in physical type.
The present study is conducted in Churachandpur town, locally known as Lamka, situated in State of Manipur, India. The required data on pregnant mothers and newborn babies were collected from the following hospitals and maternity clinics located in Churachandpur town, namely, Government District Hospital, People’s Health Foundation Trust, Sielmat Christian Hospital and Research Centre, Nazareth Nursing Home and Lamka Nursing Home. The above mentioned were the only hospitals and maternity clinics available in Churachandpur town during the study period. Of these, the state government runs only one; another are run by the Church organisations and the remaining three are run by private doctors.
The present study is based on longitudinal design conducted over a period of 16 months (November 2010-February 2012) in Churachandpur town, Manipur among the Paite tribe. To obtain the initial data, the first three months was utilized in collecting data from hospital and maternity clinics, which is later followed by visiting their respective houses till the babies attained one year of age each. Information’s on the mothers were easily collected during the consecutive house visits by personal interviewing them during the 16 months of field study. The newborns were measured within 24 hours of their birth. Thereafter, each infant was measured at monthly intervals upto the age of 12 months, with strict adherence to ±3 days at each age, by paying home visits. Hence, from birth to the age of one year each infant was weighed 13 times. For anthropometric variables, standard techniques given by Weiner and Lourie [25] were followed for both mothers and infants. The body weight of babies was accurately measured using Spring Balance Weighing Scale designed for infants with a capacity up to 20 kilogram (Figure 1). It is recorded in kilograms up to the accuracy of 20 grams. Similarly, for mothers, weight was measured to nearest 0.5 kilograms, using personal spring balance and subject with minimum possible clothing using manual bathroom weighing machine. Information about practice of Pica, food cravings and taboos was obtained from mothers.
The data is collected from 219 infants (114 boys and 105 girls) and mother pairs between November 2010 to February 2012 from Paite tribe (Churachandpur district, Manipur, India) Due to longitudinal nature of the study, likelihood of continued stay of the parents/mothers in the town for a period of atleast one year is taken into account. However, same sample size could not be maintained throughout the study owing to factors such as going back to ancestral villages; shifting to the cities for employment opportunities, unable to trace their new rented house due to unreliable mobile phone networks in the study area, etc. As a consequence, a fluctuation in the data was observed during the study period, and by the 12th months, a total of 162 infant-mother pairs continued to remain in the study. The mothers who attained full term pregnancy formed part of this study.
The ethical issues associated with the study were taken into account. The study was approved by the Department of Anthropology, Panjab University, Chandigarh, India. A prior consent was obtained from mothers so that the infant could be measured soon after birth. The consent form was prepared in English and Paite languages, and provided to the mothers for review. After a formal consent, data collection was initiated. As data was collected in hospital/clinic setting, consent was obtained from hospitals and clinic administration as well. Special care was observed during measurement of infants with respect to hygiene and careful handling of infant under the supervision of hospital/clinic staff. The data is analyzed in consultation with a statistical programmer, using Microsoft excel and SPSS 16. The results thus obtained are presented in tabular form followed with suitable interpretation.
Food practices among pregnant paite women
The food habits of the Paite are not heavy on oil and spices and yet are delicious. Rice and meat formed their staple diet. The four compulsory courses in a meal are steaming platter of steamed rice called ‘buhsi’, chutney made entirely of hot fresh chillies burned and grinned to paste with fermented animal fats called ‘sathu’ or fermented soyabean called ‘bekanthu’, boiled green vegetables called ‘antuimawl’ taken to stream down the food particles and to help in digestion and the main curry prepared with rice and dry/fresh meat over charcoal fire exuding flavor by adding some drops of distilled fresh-ash water called ‘ta-ngal’ into it, that may include braising, finally producing totally authentic curry called ‘mehpok’ served at the centre of the round plate. From table 1, it is observed that the number of frequencies varies from birth through one year of age. These are due to the above-cited reason in Pica as well as non-traceable respondents due to change of residence. The mean weight of babies born to women who practiced food taboos were 3.19 kg at birth, 7.88 kg at 6th months and 9.67 kg at 12th (Figure 2). Similarly, for mothers who do not observe taboos, the mean weight of babies are 3.25 kg at birth, 8.07 kg at 6th months and 9.78 at 1 year of age respectively. Throughout the study period, it is found that the birth weight of babies born to mothers who does not practice food taboo are relatively higher than mothers who observed taboos during their pregnancy. The most common food taboos observed among the study population are crab, jackfruit, honey, bee, yam, egg, papaya, snake meat, monkey meat, disfigured food and bitter foods. Despite embracing Christianity as their religion, it is interesting to see how culture plays a vital role in ones belief in a community. Apart from food taboos, cultural taboos, such as avoidance of hair cutting, visiting a funeral are observed by the pregnant women.
| Table 1: Mean weight and taboo | ||||
| Age (in months) |
Taboo | N | Mean weight in kg (SD) |
Std. Error Mean |
| Birth | No | 44 | 3.25(.441) | 0.066 |
| Yes | 142 | 3.19(.454) | 0.038 | |
| 6 | No | 38 | 8.04(.977) | 0.158 |
| Yes | 127 | 7.89(.842) | 0.075 | |
| 12 | No | 37 | 9.77(.835) | 0.137 |
| Yes | 125 | 9.67(.805) | 0.072 | |
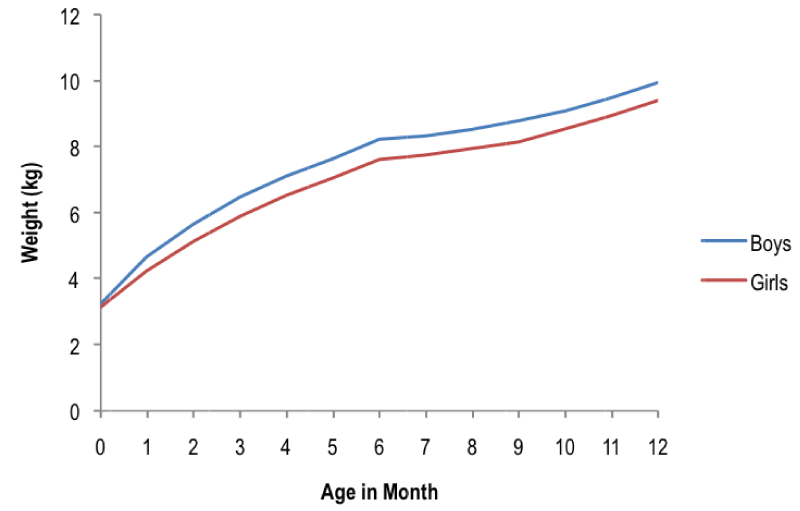
Figure 1: Distance curve for weight from birth to 12 months.
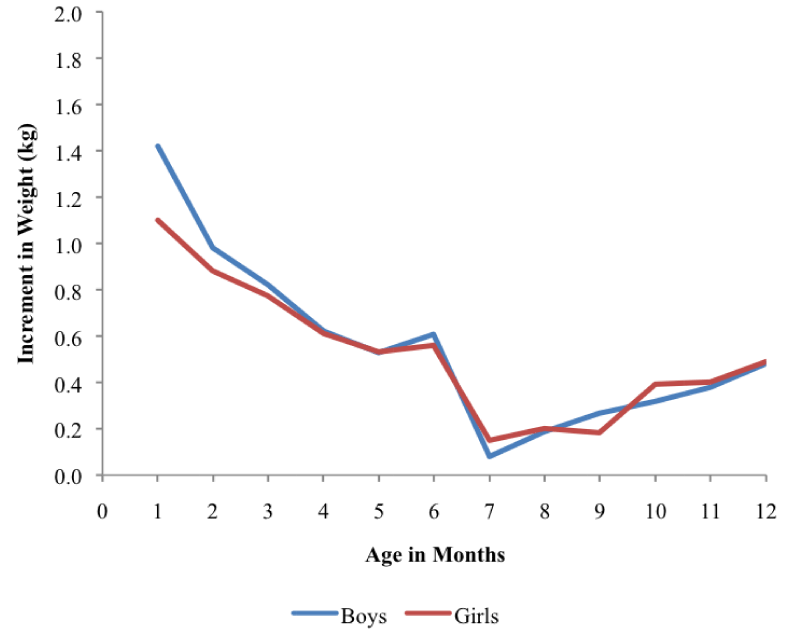
Figure 2: Velocity curve for weight from birth to 12 months.
Using students’ ‘t-test’ as shown in table 2, there was no significant difference between birth weight of babies born to mothers who observed taboo and non-observer mothers from birth through one year of age. Despite the practice of food taboos in the form of crab, jackfruit, honey, bee, yam, egg, papaya, snake meat, monkey meat, disfigured food and bitter foods, we observed that consumption of seasonal fruits, organic vegetables, fish, rice and meat are high. This may fulfill their nutritional needs created by food taboos.
| Table 2: Student’s t-test for equality of means | ||||
| Age (in months) |
t-value | df | 95% Confidence Interval of the Difference | |
| Lower | Upper | |||
| Birth | .780 | 184 | -.093 | .214 |
| 6 | .917 | 163 | -.171 | .467 |
| 12 | .647 | 160 | -.202 | .398 |
Pica was practiced by five women among the studied population as shown in table 3, in the form of charcoal, kerosene oil, and ash. The mean birth weight of women practicing pica was 2.84 kg. It is observed that the mean birth weight of babies born to mothers practicing pica is comparatively very less when compared to the overall mean birth weight in the present study. These five babies, however, were not possible to be followed till they attained the age of 1 year due to various complications in their health. On the other hand, most of the pregnant women studied enjoyed food cravings of different kinds during their pregnancy. The most common food cravings observed are mostly sour fruits, meat and in few cases local bidi.
| Table 3: Prevalence of ‘Pica’ and birth weight | ||
| Maternal characteristics | N | Mean weight at birth (kg) |
| Pica practice | 5 | 2.84 |
| Total | 186 | 3.19 |
Longitudinal weight gain of infants
It can be summarized from table 4 that the mean weight of the babies are 3.19kg, 7.92 kg and 9.69 kg at birth, 6th and 9th months respectively. The longitudinal mean weight gain of both girls and boys from birth through one year of age is shown in tables 4, 5 and 6. The mean weight of the girl babies at birth is 3.14 kg with the values ranging between 2.00 and 4.50 kg. It is observed that the mean weight of the girls increases gradually from birth till they attain the age of 1 year. The maximum increase in mean weight is observed from birth to 1 month (35%), followed by 1 to 2 months (20%), and thereafter the monthly gain in mean weight reduces from 3rd till 9th month. However, from the 9th month till 12th month once again the monthly increment in mean weight shows an increase. The observed intra sample variability in weight is highest at birth and 1 month and lowest at 12 months. At the age of 1 year the lightest girl weighs 6.80 kg and the heaviest one weighs 11.50 kg.
| Table 4: Mean weight of the babies | ||
| Mean weight at birth (kg) | Mean weight at 6th months (kg) | Mean weight at 12th months (kg) |
| 3.19 | 7.92 | 9.69 |
| Table 5: Mean weight of girls from birth to 12 months of age | |||
| Age (months) |
N | Mean (kg) |
±SD |
| Birth | 105 | 3.14 | 0.45 |
| 1 | 88 | 4.24 | 0.60 |
| 2 | 83 | 5.12 | 0.64 |
| 3 | 80 | 5.89 | 0.63 |
| 4 | 79 | 6.50 | 0.64 |
| 5 | 78 | 7.03 | 0.69 |
| 6 | 77 | 7.59 | 0.71 |
| 7 | 76 | 7.74 | 0.73 |
| 8 | 75 | 7.94 | 0.75 |
| 9 | 75 | 8.12 | 0.82 |
| 10 | 74 | 8.51 | 0.72 |
| 11 | 74 | 8.91 | 0.74 |
| 12 | 74 | 9.40 | 0.75 |
| Table 6: Mean weight of boys from birth to 12 months of age | |||
| Age (months) | N | Mean (kg) | ±SD |
| Birth | 114 | 3.24 | 0.45 |
| 1 | 99 | 4.66 | 0.65 |
| 2 | 93 | 5.64 | 0.71 |
| 3 | 92 | 6.46 | 0.72 |
| 4 | 91 | 7.08 | 0.76 |
| 5 | 88 | 7.61 | 0.81 |
| 6 | 88 | 8.22 | 0.89 |
| 7 | 88 | 8.30 | 0.84 |
| 8 | 87 | 8.49 | 0.83 |
| 9 | 88 | 8.76 | 0.78 |
| 10 | 88 | 9.08 | 0.75 |
| 11 | 88 | 9.46 | 0.76 |
| 12 | 88 | 9.94 | 0.77 |
Similarly, the average mean birth weight of the boys is 3.24 kg wherein the value ranges between 2.20 and 4.50 kg. The average mean weight of boys increases gradually from birth till 1 year of age, with maximum gain occurring between birth and 1 month (43.8%) followed by 1-2 months (21.03%). The least gain in mean weight of boys is observed from 6-7 months (0.9%). The intra sample variability shows a trend similar to that observed for girls. At the age of 1 year the difference between lightest boy (8.20 kg) and the heaviest boy (11.70 kg) is much less as compared to that observed among girls. An attempt has been made to find the correlation between mothers’ weight and infant growth. The mean weight of the 219 mothers at the 9th month of pregnancy is 57.84 kg (±7.66), with the values ranging between 42- 80 kg.
The correlation values as listed in table 7 show that in both boys and girls the birth weight is significantly correlated with mothers’ weight. Table 8 gives the correlation values between mothers’ weight and growth of boys and girls at the age of 12th months. This has been done to understand whether the correlations observed at birth are similar or different than the correlations between various measurements at 12th months of growth of infants.
| Table 7: Correlations between mother and infant anthropometric variables at birth | ||
| Infant Variable |
Girls n= 105 |
Boys n= 114 |
| Mothers n=219 | Mothers n=219 | |
| Weight (kg) | Weight (kg) | |
| Weight (kg) | 0.249* | 0.244** |
| **- significant at the 0.01 level; *-significant at the 0.05 level | ||
| Table 8: Correlations between mother and infant anthropometric variables at 12th month | ||
| Infant Variable | Girls n=74 | Boys n=87 |
| Mothers n=219 | Mothers n=219 | |
| Weight (in kg) | Weight (in kg) | |
| Weight (kg) | 0.279* | 0.222* |
| **- significant at the 0.01 level; *-significant at the 0.05 level. | ||
According to WHO [26], the normal birth weight for babies is 2.5 kg. In the present study, the mean birth weight is 3.14 kg for girls and 3.24 kg for boys. It is observed from previous studies on infants [27,28] that infants double their birth weight at the 5th month and triple it by one year of age. Among the present study population, an almost similar growth pattern was observed. The infants double their birth weight at the age of 4th months and triple it by one year of age that is also in accordance with the findings among Punjabi upper class infants of Chandigarh [29]. The growth pattern follows a similar trend for both boys and girls, with boys having a higher weight values from birth to 1 year of age. According to Meredith [30], body growth is much more rapid during the first 6 months after birth than during the succeeding 6 months. A similar trend of growth was observed in the present study population. A comparison was made with other studies working on longitudinal growth of infants during the first year of life with measurements conducted on monthly intervals. The compared populations are Punjabi infants of Chandigarh [29]; Kannada infants of Karnataka [31]; infants of Lodha tribes and non-Lodha of West Bengal [32].
The mean weight of the babies from birth through one year of age among the Paite infants are found higher than the other populations considered. An average gain from birth to 6 months among the present study population is 4.98 kg in boys and 4.45 kg in girls. Among the compared population, the average gain during the first 6 months is 3.5 kg for both boys and girls among the Karnataka infants; 2.74 and 2.95 kg for boys and girls among the Lodha tribe of west Bengal; 3.34 and 3.09 kg for boys and girls of Non-Lodha of West Bengal; 4.41 and 4.01 for boys and girls of Punjabi. In all the populations, we observed that boys mean weight are heavier than their counterparts at all stages, however among the Lodha tribes the average gain from birth to 6 months of age was higher among the girls babies. The slowing of infancy growth rates between 6 and 12 months is observed among all the populations.
A number of studies have been carried out to find out the correlations between maternal and infant anthropometric variables at birth [2,33,34]. However, data on the correlations based on longitudinal series are limited to find. Newmann et al. [1] in their studies on the influence of maternal anthropometric variables among the rural Kenya infant from birth to 6 months observed that maternal weight (for all three trimesters) were positively correlated with infant weight, length and MUAC. An attempt has been made in the present study to find the correlation between mothers’ weight and infants birth weight and weight gain. The birth weight of boys and girls is significantly correlated with mothers’ weight. This finding is supported by certain previous studies [4,6,35,36]. It is rare to find previous studies on relationship between maternal anthropometry and infants at the 12th months of age. Further, Pearson correlation was applied in order to find any significant influence of maternal weight at the 9th month of pregnancy on longitudinal series of weight gain. It is observed that maternal weight during the 9 month of pregnancy has a significant influence on the weight gain of infants during their entire first life. It would be interesting to carry further research work to find whether maternal weights still have influence or association on the babies with the advancing of age.
Among the Paite, prevalence of pica is found to be low as compared to studies conducted in the Sub-African countries [37,38]. There is however no known reasons behind how some women develop pica cravings during pregnancy. According to Rainville [39], pica cravings may somewhat be directly related to iron deficiency. While, some hypothesize that pica cravings are the body’s attempt to obtain vitamins or minerals that are missing through normal food consumption. It is observed that the mean birth weight of babies born to mothers who practice pica was very low than the birth weight of their counterparts. However, it is not possible to generalise due to the small frequency of pica practicing mothers. According to Rainville [39], a study conducted surveying medical records in Houston and Prairie View, Tex. Medical records, observed no differences in mean birth weight of infants born to women from pica practiced group and the non pica group. However, Khousabi et al. [40] found that pica has adverse effects on pregnancy outcomes in Iran. Kariuki et al. [41] among the Western Kenyan pregnant women, observed pica prevalence at 27.4%, with consumption of soil and soft stones being frequently reported. Apart from these, a number of studies on pica practice were prevalent among pregnant women across sub-Saharan countries such as Kenya, Ghana, Rwanda, Nigeria, Tanzania and South Africa [37,38].
It is interesting observation that no significant difference between mean weight of babies from birth through the age of 1 year between mothers who practice food taboos and non-observer. However, it is found that, the mean weight of the babies throughout the study was comparatively higher among non-taboo observer. The high intake of meat, fish, seasonal fruits and vegetables could be one of the main factors behind no observance of significant difference between mothers of both taboo observer and non-observer. Some researchers have suggested that a dietary pattern characterized by high intake of vegetables, plant foods, and vegetable oils decreases the risk of preeclampsia [42]. In contrast to the present findings, Lakshmi [43-46], made a study among the tribal women of Srikakulam district of Andhra Pradesh. She observed that, food taboo results in Protein Energy malnutrition and other deficiencies in women thus causing complications to both the mother and the child [47-50].
Based on findings from the present study, it can be concluded that, pica cravings, which can lead to adverse birth outcomes need more attention. This practice must be taken into account by healthcare providers to assess the nutritional status and dietary patterns of the pregnant women. For women practicing Pica, special counseling sessions must be held to educate them about balanced diet, healthy food and importance of their nutrition for growth of their child. With respect to weight of the infant, it would be interesting to carry further research work to find whether maternal weights still have influence or association on the babies with the advancing of age.
- Neuman C, Ferguson L, Bwibo NO. Maternal anthropometry as a risk predictor of pregnancy outcome: The nutrition CRSP in Kenya. Bull World Health Organ. 1995; 73: 91-95. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20604500
- Karim E, CGN Mascie-Taylor. The association between birthweight, socio-demographic variables and maternal anthropometry in an urban sample from Dhaka, Bangladesh. Ann Hum Biol. 1997; 24: 387-401. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9300116
- Nahar S, Mascie-Taylor CG, Begum HA. Maternal anthropometry as a predictor of birth weight. Public Health Nutr. 2007; 10: 965-970. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17686192
- Elshibly EM, Schmalisch G. The effect of maternal anthropometric characteristics and social factors on gestational age and birth weight in Sudanese newborn infants. BMC Public Health. 2008; 8: 244. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2522375/
- Tan, K, G Yeo. Influence of maternal height, weight and body Mass Index on Birthweight in an Asian Population. The Internet Journal of Gynecology and Obstetrics. 2009; 11.
- Ugwa EA. Maternal anthropometric characteristics as determinants of birth weight in North‑West Nigeria: a prospective study. Nigerian Journal of Basic and Clinical Sciences. 2014; 11: 8-12.
- Colding J, Folke C. The relations among threatened species, their protection, and taboos. Ecol Soc. 1997; 1: 6.
- Manderson L, Mathews M. Vietnamese attitudes towards maternal and infant health. Med J Aust. 1981; 1: 69-72. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7231251
- Trigo M, Roncada MJ, Stewien GT, Pereira IM. Food taboos in the northern region of Brazil. Rev Saude Publica. 1989; 23: 455-464. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/2641837
- Mitchell J, Mackerras D. The traditional humoral food habits of pregnant Vietnamese–Australian women and their effect on birth weight. Aust J Public Health. 2010; 19: 629-633. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8616205
- UNICEF. Strategy for improved nutrition of children and women in developing countries. New York: UNICEF. 1990.
- Cooksey NR. Pica and olfactory craving of pregnancy: How deep are the secrets? Birth. 1995; 22: 129–135. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7575860
- Horner RD, Lackey CJ, Kolasa K, Warren K. Pica practices of pregnant women. J American Dietetic Association. 1991; 91: 34–39.
- UNICEF: ChildInfo. Monitoring the Situation of Children and Women. Statistics By Area / Child Nutrition. A World Fit for Children Goal.
- Mohammadzadeh A, Farhat A, Amiri R, Esmaeeli H. Effect of Birth Weight and Socioeconomic Status on Children's Growth in Mashhad, Iran. Int J Pediatr. 2010; 1-5. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20652093
- Hien NT, Ushijima H. Nutrition status of low birthweight ethnc minority infants in Backan province, Vietnam. Pediatr Int. 2007; 49: 266-272. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17445055
- Victora CG, Adair L, Fall C, Hallal PC, Martorell R, et al. Maternal and child under nutrition: consequences for adult health and human. Lancet. 2008; 26: 340-357.
- Kossmann J, Nestel P, Herrera MG, El Amin A, Fawzi WW. Undernutrition in relation to childhood infections: a prospective study in the Sudan. Eur J Clin Nutr. 2000; 54: 463-472. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10878647
- Li H, Barnhart HX, Stein AD, Martorell R. Effects of early childhood supplementation on the educational achievement of women. Pediatrics. 2003; 112: 1156-1162. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/14595062
- Haas JD, Murdoch S, Rivera J, Martorell R. Early nutrition and later physical work capacity. Nutr Rev. 1996; 54: S41-48. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8710235
- Hoffman DJ, Sawaya AL, Verreschi I, Tucker KL, Roberts SB. Why are nutritionally stunted children at increased risk of obesity? Studies of metabolic rate and fat oxidation in shanty town children from São Paulo, Brazil. Am J Clin Nutr. 2000; 72: 702-707. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10966887
- WHO working group on infant growth. An evaluation of infant growth: the use and interpretation of anthropometry in infants. Bulletin WHO. 1995; 73: 165-174. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2486761/
- Kirchengast S, Hartmann B. Advanced maternal age is not only associated with newborn somatometrics but also with the mode of delivery. Ann Hum Biol. 2003; 30: 1-12. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12519651
- Pickett KE, Abrams B, Selvin S. Maternal height, pregnancy weight gain, and birthweight. Am J Hum Biol. 2000; 12: 682-687. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11534061
- Weiner JS, Lourie JA. Practical human biology. London: Academic Press. 1981.
- WHO. Low birth weight: a tabulation of variable information. Geneva: World Health Organization. 1992.
- Hewitt D, Stewart AD. The oxford child health survey: a study of the influence of social and genetic factors of infant weight. Human Biology 1952; 24: 309-319.
- Scott RB, Kessler AD, Clark BG, Hialt HH, Ferguson AD. Growth and development of Negro infants. Am J Diseases Children. 1959; 98: 526.
- Bhalla AK. A longitudinal study of body growth of Punjabi children during the first year of life. PhD thesis, Panjab University, Chandigarh. 1983.
- Meredith HV. North American negro infants: size at birth and growth during the first post-natal year. Human Biology. 1952; 24: 290-308.
- Khadi PB, Khateeb S, Surendra HS, Kalliguddi YS, Phadnis T. Growth of rural infants- a longitudinal study. Karnataka J Agric Sci. 1990; 3: 246-252.
- Sinha NM, Das S, Bose K, Nandi DK. A longitudinal study of weight among Lodha and non-Lodha infants and young children of Lodasuli, West Bengal, India. Antrocom Online Journal of Anthropology. 2010; 6: 135-140.
- Gogoi G, Ahmed FU. Effect of maternal nutritional status on the birth weight among women of tea tribe in Dibrugarh district. Indian Journal of Community Medicine. 2007; 32: 120-122.
- Pomeroy E, Wells JCK, Cole TJ, O’Collaghan M, Stock JT. Relationships of maternal and paternal anthropometry with neonatal body size, proportions and adiposity in an Australian cohort. Am J Phys Anthropol. 2015; 156: 625-636. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25502164
- Tabrizi FM, Sarawathi G. Maternal anthropometric measurements and other factors: relation with birth weight of neonates. Nutr Res Pract. 2012; 6: 132-137. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3349035/
- Sahu KK, Agarwal M, Ahmed M, Singh SK, Khanna A. Incidence of low birth weight and effect of maternal factors on birth weight of neonates in rural areas of Uttar Pradesh. International Journal of Multidisciplinary Research and Development. 2015; 2: 707-715.
- Al-Rmalli SW, Jenkins RO, Watts MJ, Haris PI. Risk of human exposure to arsenic and other toxic elements from geophagy: trace element analysis of baked clay using inductively coupled plasma mass spectrometry. Environ Health. 2010; 9: 79. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3022881/
- Corbett RW, Ryan C, Weinrich SP. Pica in pregnancy: Does it affect pregnancy outcomes?. MCN: Am J Matern Child Nurs. 2003; 28: 183–188. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12771697
- Rainville AJ. Pica practices of pregnant women are associated with lower maternal hemoglobin level at delivery. J Am Diet Assoc. 1998; 98: 293–296. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9508011
- Khoushabi F, Ahmadi P, Shadan MR, Heydari A, Miri A, et al. Pica Practices among Pregnant Women Are Associated with Lower Hemoglobin Levels and Pregnancy Outcome. Open Journal of Obstetrics and Gynecology. 2014; 4: 646-652.
- Kariuki L, Lambert C, Purwestri R, Biesalski HK. Trends and consequences of consumption of food and non-food items (pica). NFS Journal. 2016; 5: 1–4.
- Ademuyiwa MO, Sanni SA. Consumption pattern and dietary practices of pregnant women in Odeda local government area of Ogun state. International Journal of Agricultural, Biosystems Science and Engineering. 2013; 7: 1049-1053.
- Lakshmi G. Food preferences and taboos during ante-natal period among the tribal women of north coastal Andhra Pradesh. Journal of Community Nutrition and Health. 2013; 2: 32-37.
- Evans EC. A Review of Cultural Influence on Maternal Mortality in the Developing World. Midwifery. 2013; 29: 490-496.
- Fikentscher W. Modes of thought- a study in the anthropology of law and religion. Tubingen: Mohr Siebeck Publ. 2004.
- Kramer M. Determinants of intrauterine growth and gestation duration. Bulletin of World Health Organization. 1987; 65: 663-737.
- Mascie-Taylor CGN. Relationship of maternal anthropometry and birth outcome. BIRPHERT Research Report. Dhaka, Bangladesh. 1993.
- VanLoon H, Saverys V, Vuylsteke JP, Vlietnck RF, Eeckels R. Local versus universal growth stan- dards: The effect of using NCHS as a universal reference. Ann Hum Biol. 1986; 13: 347-357.
- Liamputtong P, Yimyam S, Parisunyakul S, Baosoung C, Sansiriphun N. Traditional Beliefs about Pregnancy and Child Birth among Women from Chiang Mai, Northern Thailand. Midwifery. 2005; 25: 139-153. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15878429
- Habicht JP, Yarbrough C, Martorell R, Malina RM, Klein RE. Height and weight standards for pre- school children. Lancet; 1974; 1: 611-615. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/4132271