More Information
Submitted: January 04, 2021 | Approved: January 08, 2021 | Published: January 11, 2021
How to cite this article: Manieri S, Mirauda MP, De Gregorio F, Colangelo C, Tagliente M, et al. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): A case with adverse reaction to three drugs alternately administered. J Adv Pediatr Child Health. 2021; 4: 001-005.
DOI: 10.29328/journal.japch.1001022
ORCiD iD: orcid.org/0000-0002-6317-3043
Copyright License: © 2021 Manieri S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Case report; DRESS syndrome; reaction adverse to three drugs
Abbreviations: DRESS: Drug Reaction with Eosinophilia and Systemic Symptoms; DiHS: Drug-Induced Hypersensitivity Syndrome; SCAR: Severe Cutaneous Adverse Reactions; CRP: C-Reactive Protein; HLA: Human Leukocyte Antigen; HVV-6: Human Herpesvirus 6; HVV-7: Human Herpesvirus 7; EBV: Epstein Barr Virus; CMV: Cytomegalovirus; IL-6: Interleukin 6; ALT: Alanine Aminotransferase; ALP: Alkaline Phosphatase; GGT: Gamma-Glutamyl Transpeptidase; ALP: Alkaline Phosphatase; LDH: Lactate Dehydrogenase; JIA: Juvenile Idiopathic Arthritis; IVIG: IntraVenous Immuno Globulin
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): A case with adverse reaction to three drugs alternately administered
Sergio Manieri*, Maria P Mirauda, Fabiola De Gregorio, Carmela Colangelo, Maria Tagliente, Rosaria Abate, Luciana Romaniello, Rosa Lapolla and Donatello Salvatore
Department of Pediatrics, San Carlo Hospital, Potenza, Italy
*Address for Correspondence: Sergio Manieri, Department of Pediatrics, San Carlo Hospital, Potenza, via Fontanelle, n° 84. 85028 Rionero in Vulture (PZ), Italy, Tel: +39 3285782056; Email: [email protected]
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a severe multiorgan hypersensitivity reaction mostly caused by several eliciting drugs in patients with a genetic predisposition. Incidence of DRESS in children is very variable, frome 1:1000 to 1:10.000, and the mortality rate seems to be lower than 10%. Anti-convulsants are the main drugs involved both in adults and in children. The treatment of choice is the prompt withdrawn of the offending drug and using intravenous immunoglobulins and corticosteroids used in synergy. In recent years, emerging studies have outlined the disease more clearly. We present a pediatric case in which the patient developed DRESS syndrome as a result of exposure to lamotrigine before and carbamazepine after and a relapse after exposure to omeprazole. Starting from this case report we provide an overview on DRESS Syndrome.
Drug reactions are characterized by a multiplicity of clinical pictures and the recognition of different pathogenetic mechanisms. Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, which is also termed drug-induced hypersensitivity syndrome (DiHS), is one of the drug-induced severe cutaneous adverse reactions (SCARs). DRESS was identified in 1966 as a distinct clinical syndrome by Bocquet, et al. [1]. The incidence of DRESS is estimated overall population risk of between 1 in 1000 and 1 in 10.000 drug exposures [2]. DRESS syndrome can have a benign and self-limiting course as well as a severe and potentially fatal course, its mortality rate is about 10%, with a lower percentage in children than in adults [3]. The clinical presentations of DRESS syndrome are characterized by fever, widespread skin lesions, internal organ involvement, a long latent period after intake of the inciting drug, a prolonged and protracted clinical course, and possible sequential reactivation of various HHVs [4]. The phenotypic variability often makes the differential diagnosis difficult both between the different types of drug reactions and with other systemic pathologies of different nature (infectious, rheumatological, neoplastic) causing therapeutic delays and possible negative prognostic.
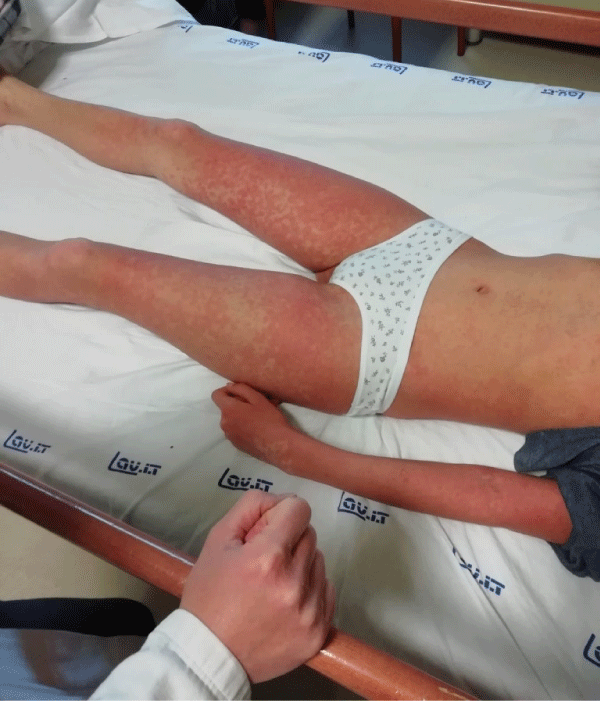
A 13 years old, female, comes to our observation for skin rash, fever, epigastralgia, marked asthenia. In anamnesis eating disorder and recent diagnosis of epilepsy (about 2 months earlier) for which he started therapy with lamotrigine. Upon reaching the full dose of the antiepileptic, the appearance of skin rash was observed (Figure 1) for which the neurologist consultant replaced lamotrigine with carbamazepine. After 4 days onset of high remitting fever with persistence of the rash and significant worsening of the general clinical condition (Figure 2). Clinically, the patient appeared febrile, dejected, with a diffuse itchy skin rash given by confluent maculo-papular skin lesions associated with perioral desquamation, oral aphthae, periorbital and face edema, angolomandibular and inguinal lymphadenopathy, regular cardiorespiratory activity, abdomen painful in the epigastric region. Laboratory tests showed increased inflammation indices (CRP, procalcitonin, IL-6), leukocytosis with eosinophilia, hypertransaminasemia, associated with elevated cholestasis indices (GGT, ALP, bilirubin), hepatic protidosynthesis deficiency (hypoalbuminemia, QT lengthening), increased LDH and D-Dimers, elevated IgE levels. The abdomen ultrasound showed hepatomegaly without focal lesions, minimal fluid flap in the perihepatic area. Arterial hypotension was also observed. He performed an echocardiogram with evidence of circumferential pericardial effusion, with an increase in troponin I. The infectious and immunological screening (C3, C4, autoantibodies) was negative. The anamnestic and laboratory clinical picture indicated a systemic reaction to drugs, such as antiepileptics. Therefore, antiepileptic therapy was suspended and IV steroid therapy was introduced, in association with omeprazole, vitamin K, albumin infusions, hydroelectrolytic support. Close clinical, laboratory and cardiological monitoring was carried out. There was a gradual clinical improvement (gradual involution of the skin rash, lymphadenopathy, defervescence, reduction of asthenia) and laboratory (reduction of inflammation indices, troponin, normalization of liver function) and echocardiography (reduction of pericardial effusion). After 3 days of apyrexia, resumption of fever and re-ignition of the skin rash was observed (Figure 3). In the suspicion of a recovery of the clinical picture from a reaction to drugs in use, omeprazole was suspended and replaced with ranitidine, observing a subsequent involution of the clinical picture. The young patient is still in close clinical-laboratory follow-up.
Figure 1: Skin rash caused by Lamotrigine.
Figure 2: Skin rash caused by Carbamazepine.
Figure 3: Skin rash caused by Omeprazole.
Dress Syndrome is a life-threatening disease with cutaneous presentation and internal organ involvement [5]. Skin lesions in patients with DRESS syndrome are most prevalente, they present in 73% – 100% of the patients [5]. Typically, skin rash are generally not specific and involves more than half of the body surface area and the cutaneous lesions are frequently of polymorphic presentations such as macupapular, urticarial, exfoliative, lichenoid, pustular, bullous, target-like, or eczema-like lesions. Mucosal lesions are reported in more than 50% of DRESS cases [6]. Regarding the organic systems and solid organs involved, Eosinophilia is the most common hematological abnormalities, being present in 66% – 95% of patients [2,6]. Similar with eosinophils, atypical lymphocytes and lymphadenopathy are present [6]. Liver injury is the most common type of organ damage and has been found in 75% – 94% of patients [2,6]. This damage can occur before the skin lesions appear and tends to be very severe and last a long time [7]. Liver injury is divided into three different types: cholestatic type, hepatocellular type, and mixed type [8]. This determination is based on the values of alanine aminotransferase (ALT) and alkaline phosphatase (ALP) at the initial presentation. Pulmonary involvement may present with acute respiratory distress syndrome, impaired pulmonary function, interstitial pneumonitis and pleuritis [9], it is quite frequent occurring in about one-third of DRESS patients [6]. Renal involvement is also prevalent in patients with DRESS syndrome, occurring in around 12% – 40% of patients [2,6], but is usually mild. However, in some cases, acute tubular necrosis, severe interstitial nephritis and renal vasculitis could develop and may lead to renal failure or even mortality [9]. Cardiac involvement is less frequent, has been reported in 4% – 27% [10] and usually it is left ventricular dysfunction and electrocardiographic changes [11]. Cardiac involvement includes two forms of reactions: a) acute necrotizing eosinophilic myocarditis, that is a more severe form of hypersensitivity and results in rapid deterioration with a high mortality rate of more than 50% [11], b) hypersensitivity myocarditis, that is usually mild and self-limited. In our case occurred circumferential pericardial effusion, with an increase in troponin I. Less frequenttly there are neurologic manifestations include headache, seizure, coma, and motor function impairment. These may result from meningitis or encephalitis [12]. Finally, the involvement of other organs is occasionally encountered, including the pancreas, gastrointestinal tract, and spleen [2,6].
The diagnosis of DRESS syndrome requires careful clinical observations and a thorough laboratory examination. The most used diagnostic criteria are included in the scoring system proposed by the RegiSCAR group [13,14]. This scoring system comprises the major features of DRESS syndrome, giving each item a score of minus one point, zero points, one point, or two points. The diagnosis of DRESS syndrome is then made based on the total score: < 2 points: no case; 2–3 points: possible case; 4–5 points: probable case; >5 points: definite case (Table 1).
| Table 1: The RegiSCAR scoring system for diagnosing DRESS syndrome. | |||
| RegiSCAR Diagnosis Score for DRESS | |||
| Features | No | Yes | Unknown |
| Fever (> 38.5°C) | -1 | 0 | -1 |
| Enlarged lymph nodes (> 2 sites, > 1 cm) | 0 | 1 | 0 |
| Atypical Lymphocytes | 0 | 1 | 0 |
| Eosinophilia 700-1499 or 10% - 19.9% > 1500 or > 20% |
0 | 1 2 |
0 |
| Skin Rash Extend > 50% At least 2: edema, infiltration, purpura, scaling Biopsy suggesting DRESS |
0 0 -1 -1 |
1 1 0 |
0 0 0 0 |
| Internal Organ Involvement One Two or more |
0 |
1 2 |
0 |
| Resolution in more than 15 days At least 3 biological investigations done and negative to exclude alternative diagnosis |
-1 0 |
0 1 |
-1 0 |
| Final score: < 2 = no; 2-3 = possible; 4-5 = probable; > 5 = definite | |||
The pathomechanisms of DRESS syndrome is not simple, but it is the result of a complex interplay of drugs, genetic factors, immunological response, reactivation of herpes virus family members (HHV-6 and HHV-7, EBV and CMV) [3]. Many drugs have been reported to be a causative agent of DRESS syndrome (Table 2). The most peculiar feature of these culprits is a long latent period, which ranges from 3 to 8 weeks after commencement of the drugs [2]. Only a limited number of drugs are frequently encountered as culprits, while several newly developed drugs have also been reported as DRESS syndrome culprits. This means that with increasing introdutions of new drugs the list of culprit drugs for DRESS syndrome will continue to grow [2]. Patients with DRESS syndrome typically develop symptoms and signs of drug reaction at least 3 weeks after the start of the eliciting drug. The duration of illness of DRESS syndrome is usually more than 15 days, with waxing-and-waning quality in which several flare-ups may occur after recovery from the initial presentation [2]. There is evidence of disease recurrence after using a structurally unrelated new drug within an unusually short period of time, with more than 50% of those cases having more than one episode [15]. The exact pathomechanism of these recurrences are still unknown. Cross-reactivity is one of the possible explanations for this phenomenon.
| Table 2: The common culprit drugs in DRESS syndrome. | |
| Category | Drugs |
| Anti-convulsants | Lamotrigine, valproic acid, Carbamazepine, oxacarbamazepine, phenobarbital, phenytoin, levetiracetam, gabapentin, sulthiame, perampanel, rufinamide, zonisamide. |
| Anti-bacterial | Amoxicillin, amoxi-clav, ampicillin, ampicillin-sulbactam, penicillin, oxacillin, clindamycin, minocycline, cefotaxime, ceftriaxone, cefixime, cefepime, cefdinir, cefditoren-pivoxil, azithromycin, clarythromycin, levofloxacin, piperacillin/tazobactam, vancomycin, tobramycin |
| Sulfonamides | Dapsone, sulfamethoxazole-trimethoprim, sulfasalazine |
| Anti-tuberculosis | Ethambutol, rifampin, pyranzinamide, isoniazid, streptomycin |
| Anti-hepatitis C virus agents | Boceprevir, telaprevir |
| Anti-retroviral agents | Abacavir, nevirapine |
| Targeted therapeutic agents | Sorafenib, vismodegib, vemurafenib, Allopurinol, imatinib, infliximab, canakinumab, anakinra |
| Anti-pyretic/analgesics | Acetaminophen, diclofenac, celecoxib, ibuprofen, naproxen, acetylsalicylic acid, paracetamol |
| Others | mexiletine, esomeprazole, omeprazole, strontium ranelate, pyrimethamine, hydroxychloroquine, griseofulvine, fluoxetina, oxymetazoline nasal spray |
A number of emerging studies have revealed associations between drugs, polymorphisms in human leukocyte antigens (HLA) alleles and the development of DRESS syndrome. The polymorphism in genes encoding metabolizing enzymes for drugs cause the accumulation of drugs or their active metabolites, which can then interact with cellular proteins or peptides, in turn evoking immune responses [2]. Polymorphisms in HLA alleles largely explain the genetic predisposition of patients with DRESS syndrome. In fact, it has been found that DRESS syndrome is associated with certain HLA alleles [2,3] (Table 3).
| Table 3: Associations between Drugs, HLA alleles and DRESS Syndrome. | |
| Drug | Associated HLA alleles |
| Lamotrigine | A* 24:02 |
| Carbamazepine | A*31:01, A*11; B* 51 |
| Phenytoin | B*13:01, B*51:01; B*15:13, CYP2C9*3 |
| Dapasone | B*13:01 |
| Abacavir | B*57:01, DRB1*01:01, B*35:05 |
| Allopurinol | B* 58:01 |
| Nevirapine | DRB1*01:01, DRB1*01:02; Cw*4; B*35; C*04:01 |
Viral reactivation, especially HHV-6 reactivation, is an important and characteristic feature in patients with DRESS syndrome. But the role of viruses in the pathogenesis of DRESS is unclear [3]. The most common hypothesis is that the immunologic response to drugs induces a boost viral reactivation, consequently T lymphocytes and monocytes/macrophages release viruses that represents as an early marker of stimulation of these cells, rather than the triggering event in the pathogenesis of DRESS [16]. In particular, toxic drug metabolites accumulation provoke an immunosuppression of B cells with hypogammaglobulinemia and subsequent viral re-activation [17].
The mainstay treatment for patients with DRESS syndrome are systemic corticosteroids. Of course the therapy uses first of all the immediate withdrawal of the inciting drug of the syndrome. A starting dose of prednisolone or an equivalent of 0.5–1.0 mg/kg/day with a gradual tapering over 2–3 months has been suggested [18]. However, systemic corticosteroids may be associated with a higher rate of opportunistic infections and with the possibility of lots of complications. Therefore, systemic steroids may not be required for the treatment of mild forms of DRESS syndrome and should be reserved for those with severe presentations. Some authors recommend to use systemic corticosteroids when presence of 5-folds elevation of serum transaminase levels, or involvement of either other organs, such as kidney, lung, and heart [19]. Only supportive care, like hydration with or without topical steroids, may also be an option in the treatment of patients with mild forms of DRESS syndrome [20]. Intravenous immunoglobulin (IVIG) is another treatment option that has yielded conflicting results. Therefore, some authors suggested that IVIG should not be used as monotherapy in treating DRESS syndrome, but associating it with corticosteroids. Several immunosuppressive agents other than corticosteroids have been reported to exhibit treatment effectiveness, including cyclosporine, cyclophosphamide, mycophenolate mofetil, and rituximab [2]. Anti-viral treatment such as ganciclovir has been proposed in addition to systemic corticosteroids or IVIg to be used in patients with severe disease with confirmation of viral reactivation.
DRESS Syndrome is a rare (about 1/10,000) and severe drug reaction with systemic symptoms and hypereosinophilia also known as drug hypersensitivity syndrome (DiHS), characterized by high morbidity and potentially fatal (10% mortality), which requires prompt recognition and treatment. Typically associated since its earliest descriptions with antiepileptic drugs in predisposed patients (HLA): in fact, also in our case the symptoms were triggered by the administration of two antiepileptic drugs (lamotrigine before and carbamazepine after). However, it can be induced by different categories of drugs (antibiotics, antituberculosis, antivirals, antipyretics, analgesics, anticancer drugs, other drugs such as omeprazole, hydroxychloroquine, etc.). Furtheremore, in our case there was a recurrence of symptoms immediately after the introduction of omeprazole, probably because the pathophysiological mechanisms had already been activated by the two antiepileptic drugs used, with a probable mechanism of cross reactivity. It is well known that aromatic anticonvulsants, such as lamotrigine ad carbamazepine, show cross-reactivity in 40% - 80% of cases [3].
Sometimes it occurs in association with infectious triggers (Herpes virus) that can influence its severity and recurrence (which is observed in up to 25% cases). Fever, skin rash, eosinophilia, lymphadenopathy and organ involvement are the main clinical features. The liver is the most affected organ (75% - 94% cases), while cardiac involvement is observed only in a small percentage of cases (4% - 27%), as in the case described. Myocarditis is often fatal and underdiagnosed and requires immediate recognition. The severity of the clinical situation requires a rapid differential diagnosis with other hypersensitivity diseases, infectious or rheumatological diseases. The key therapy of DRESS syndrome still remains the suspension of the trigger drug and the introduction of steroids, possibly associated with IVIG and/or with several immunosuppressive agents such as Cyclosporine, cyclophosphamide, mycophenolate mofetil and rituximab. Antivirals has been proposed in the most severe cases or associated with viral infection.
- Bocquet H, Bogot M, Roujeau JC. Drug-induced pseu- dolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996; 15: 250-257. PubMed: https://pubmed.ncbi.nlm.nih.gov/9069593/
- Yung-Tsu Cho, Che-Wen Yang and Chia-Yu Chu. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): An Interplay among Drugs, Viruses, and Immune System. Int J Mol Sci. 2017; 18: 1243. PubMed: https://pubmed.ncbi.nlm.nih.gov/28598363/
- Mori F, Caffarelli C, Caimmi S, Bottau P, Liotti L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS) in children. Acta Biomed. 2019; 90: 66-79. PubMed: https://pubmed.ncbi.nlm.nih.gov/30830064/
- Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, et al. The DRESS syndrome: A literature review. Am J Med. 2011; 124: 588–597. PubMed: https://pubmed.ncbi.nlm.nih.gov/21592453/
- Peyrière H, Dereure O, Breton H, Demoly P, Cociglio M, et al. The Network of Pharmacovigilance Centers. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: Does a DRESS syndrome really exist? Br J Dermatol. 2006; 155: 422–428. PubMed: https://pubmed.ncbi.nlm.nih.gov/16882184/
- Kardaun SH, Sekula P, Valeyrie-Allanore L, Liss Y, Chu CY, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): An original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013; 169: 1071–1080. PubMed: https://pubmed.ncbi.nlm.nih.gov/23855313/
- Lee T, Lee YS, Yoon SY, Kim S, Bae YJ, et al. Characteristics of liver injury in drug-induced systemic hypersensitivity reactions. J Am Acad Dermatol. 2013; 69: 407–415. PubMed: https://pubmed.ncbi.nlm.nih.gov/23632341/
- Danan G, Benichou C. Causality assessment of adverse reactions to drugs-1. A novel method based on the conclusions of international consensus meetings: Application to drug-induced liver injuries. J Clin Epidemiol. 1993; 46: 1323–1330. PubMed: https://pubmed.ncbi.nlm.nih.gov/8229110/
- Kano Y, Ishida T, Hirahara K, Shiohara T. Visceral involvements and long-term sequelae in drug-induced hypersensitivity syndrome. Med Clin N Am. 2010; 94: 743–759. PubMed: https://pubmed.ncbi.nlm.nih.gov/20609861/
- Thongsri T, Chularojanamontri L, Pichler WJ. Cardiac involvement in DRESS syndrome. Asian Pac J Allergy Immunol. 2017; 35: 3–10. PubMed: https://pubmed.ncbi.nlm.nih.gov/27996289/
- Bourgeois GP, Cafardi JA, Groysman V, Hughey LC. A review of DRESS-associated myocarditis. J Am Acad Dermatol. 2012; 66: e229–e236. PubMed: https://pubmed.ncbi.nlm.nih.gov/21658796/
- Ozisik L, Tanriover MD, Saka E. Autoimmune limbic encephalitis and syndrome of inappropriate antidiuretic hormone secretion associated with lamotrigine-induced drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Intern Med. 2016; 55: 1393–1396. PubMed: https://pubmed.ncbi.nlm.nih.gov/27181555/
- Kardaun SH, Sidoroff A, Valeyrie-Allanore L, Halevy S, Davidovici BB, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: Does a DRESS syndrome really exist? Br J Dermatol. 2007; 156: 609–611. PubMed: https://pubmed.ncbi.nlm.nih.gov/17300272/
- Chen YC, Cho YT, Chang CY, Chu CY. Drug reaction with eosinophilia and systemic symptoms: A drug-induced hypersensitivity syndrome with variable clinical features. Dermatol Sin. 2013; 31: 196–204. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5486066/
- Picard D, Vellar M, Janela B, Roussel A, Joly P, et al. Recurrence of drug-induced reactions in DRESS patients. J Eur Acad Dermatol Venereol. 2015; 29: 801–804. PubMed: https://pubmed.ncbi.nlm.nih.gov/24628777/
- Roujeau JC, Dupin N. Virus Reactivation in Drug Reaction with Eosinophilia and Systemic Symptoms (Dress) Results from a strong drug-specific immune response. J Allergy Clin Immunol Pract. 2017; 5: 811-812. PubMed: https://pubmed.ncbi.nlm.nih.gov/28483323/
- Yazicioglu M, Elmas R, Turgut B, Genchallac T. Association between DRESS and the diminished numbers of peripheral B lymphocytes and natural killer cells: Peripheral B lymphocytes and NK cells in DRESS. Pediatr Allergy Immunol. 2012; 23: 289-296. PubMed: https://pubmed.ncbi.nlm.nih.gov/22432939/
- Shiohara T, Kano Y. Drug reaction with eosinophilia and systemic symptoms (DRESS): Incidence, pathogenesis, and management. Expert Opin Drug Saf. 2017; 16: 139–147. PubMed: https://pubmed.ncbi.nlm.nih.gov/27936971/
- Descamps V, Ben Said B, Sassolas B, Truchetet F, Avenel Audran M, et al. Management of drug reaction with eosinophilia and systemic symptoms (DRESS). Ann Dermatol Venereol. 2010; 137: 703–708. PubMed: https://pubmed.ncbi.nlm.nih.gov/21074653/
- Uhara H, Saiki M, Kawachi S, Ashida A, Oguchi S, et al. Clinical course of drug-induced hypersensitivity syndrome treated without systemic corticosteroids. J Eur Acad Dermatol Venereol. 2013; 27: 722–726. PubMed: https://pubmed.ncbi.nlm.nih.gov/22540194/