More Information
Submitted: March 12, 2021 | Approved: March 24, 2021 | Published: January 25, 2021
How to cite this article: Woldegebriel A, Beyero M, Daba AK. Factors associated with zinc prescription practice among children with diarrhea who visited public health facilities in Addis Ababa, Ethiopia: A cross sectional study. J Adv Pediatr Child Health. 2021; 4: 027-032.
DOI: 10.29328/journal.japch.1001026
Copyright License: © 2021 Woldegebriel A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Children; Diarrhea; Zinc prescription; Willingness to pay
Factors associated with zinc prescription practice among children with diarrhea who visited public health facilities in Addis Ababa, Ethiopia: A cross sectional study
Abenezer Woldegebriel1*, Mesfin Beyero2 and Alemneh Kabeta Daba3
1Amref Health Africa, Addis Ababa, Ethiopia
2Charlotte, North Carolina Area, USA
3School of Nursing, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
*Address for Correspondence: Abenezer Woldegebriel, Amref Health Africa, Addis Ababa, Ethiopia, Tel: +251912245194; Email: [email protected]
Background: Diarrhea and nutrient deficiency worsen each other, and zinc is recommended to be included in clinical management of diarrhea. Therefore, this investigation was done to assess zinc prescription practice to children with diarrhea, identify factors associated with zinc prescription, and assess caregivers’ zinc’s perceived cost and willingness to pay for.
Methods: A health institution based cross-sectional study was done. Caretakers of 609 children with diarrhea attending health centers in Addis Ababa were included. Logistic regression was applied to identify variables associated with zinc prescription.
Results: Zinc was prescribed to 62.1% of children. About 74.9% of the caregivers were willing to pay for zinc. Previous use of zinc (AOR = 2.3; 95% CI: 1.34-4.01), exposure to zinc related message (AOR = 2.6, 95% CI: 1.53-4.60) and willingness to pay for zinc (AOR = 6.9; 95% CI: 3.84-12.66) were associated with zinc prescription.
Conclusion: Zinc was not administered to considerable proportion of children with diarrhea. Previous use of zinc, exposure to zinc related message and willingness to pay for positively contributed to zinc prescription. Health care workers shall be encouraged on zinc prescription. Intervention to increase willingness to pay for zinc and zinc benefit communication shall be strengthened in parallel with operational researches.
According to World Health Organization’s (WHO) diarrhea is defined as passage of frequent watery or loose stool at least 3 times in 24 hours [1]. The disease is multifactorial and affects considerable number of children. Globally, every year about 1.7 million diarrheal cases and 525, 000 deaths are estimated [2]. Rotavirus has been recognized as a common infectious agent, and it has been addressed through the provision of vaccine to children through the routine immunization program. Though prevention and treatment modalities are there to manage diarrheal cases, it continued significantly to contribute for underfive children mortality. About 22% of mortality among under-five children was attributed to diarrhea [3]. Ethiopia is one of the top five countries accounted for high burden of under-five diarrheal deaths [4].
Zinc is a micro-mineral with a range of health benefits [5]. It is one of the public health important micronutrients [6]. Animal source foods, sea animal based flesh foods and legume crops are food items that can serve as good sources of zinc [7]. Land locked countries like Ethiopia are not naturally favored for sea foods. In the country the consumption of animal source foods is far lower than developed countries [8]. It is also documented that small proportions of Ethiopian children consumed animal source foods [9-11]. Unless household level implementable food processing techniques like soaking, germination and fermentation are well practiced, bioavailability of micronutrients in grains including legumes/pulse crops was confirmed to be low for that they contain antinutritional factors [12]. But pulse/legume crop processing practices were recommended for further study [13] and they were under promotion [14,15]. Evidence also figured out that complementary foods in Ethiopia were short of providing zinc to the level that growing children require [16].
Illness and nutrition status affect each other [17]. Likewise, diarrhea can happen and get worsen because of nutritional derangements, and it can also lead to nutritional deficiencies [18]. Accordingly, World Health Organization (WHO) and United Nations Children Fund (Unicef) recommended the inclusion of zinc in the treatment of childhood diarrhea [19]. However, evidences are limited on zinc prescription practice, perceived cost and willingness to pay for and related factors. Therefore, the purpose of the current study was to assess zinc prescription practice and identify related factors among children with diarrhea who visited public health institutions in Addis Ababa, Ethiopia.
Study area, design and period
The study was conducted in Addis Ababa city administration, Ethiopia. Based on the 2007 census, the population of Addis Ababa was counted to be 3,384,569 million [20]. Addis Ababa city has a total of 10 sub-cities and 86 health centers. A cross-sectional epidemiologic study design was applied. The study was conducted from September 23- November 20, 2015.
Sampling
Sample size was determined using a single population proportion formula [21] considering 95% confidence level, 50% proportion, 1.5 design effect and 10% non-response rate. Multi-stage sampling technique was employed to reach at the study unit level. Two health centers were selected from each of the five selected sub-cities. The selection of both sub-cities and health center was on lottery bases. A total of 633 under-five children with diarrhea were included in the study who attended the selected health centers.
Data collection
Data were collected using a pre-tested semi-structured questionnaire. The tool consisted of questions on socio-demographic and economic characteristics, and zinc and related issues relevant to the objectives of the investigation. Eight trained data collectors and two supervisors participated in the data collection process. Data were collected through one-on-one interview.
Data management
Each questionnaire was checked for completeness, missing values and unlikely responses and cleaned manually. Questionnaires judged incomplete were excluded from analysis. Data entry was performed using Epi Info version 7 and analyses was performed using SPSS version 20.0 software. During data analysis sorting was used to check for missed variables, outliers and other errors. Descriptive statistical analyses were carried out to generate summary figures on the socio-demographic and demographic characteristics and zinc related outcomes. Bivariate and multivariable logistic regression analyses were done to identify factors associated with zinc prescription. Significance of results was decided at p - value of 0.05.
Sociodemographic and economic characteristics
The study was done on a total of 633 under five children. Twenty four (n = 24) incomplete data cases were excluded from analysis. Slightly more than half, 334 (54.8%), of the children were males. Children’s mean age was 19.5 months.
Majority, 474(77.8%), of the respondents were children’s mothers. They were from multiple ethnic backgrounds: 221 (26.8%) Amhara, 163(26.8%) Oromo, 120(20%) Gurage and 97(15.9%) Tegaru. By religion, majority (62.1%) of the respondents were Orthodox Christians. Concerning their education status, 106(17.4%) cannot read and write, 179 (29.47) attended primary/elementary school, 157(25.8%) attended high school, 98(16.1%) attained college diploma and the remaining 69 (11.3%) were with bachelor degree and above. Nearly three-fourth (72%) of the participants was from households with 2000 Ethiopian Birr (ETB) or less average monthly income (Table 1).
| Table 1: Sociodemographic and economic characteristics of the study participants. | ||
| Variable | N (%) | |
| Child Sex | Male | 334(54.8%) |
| Female | 275(45.2%) | |
| Child Age | ||
| Caregivers’ Religion | Orthodox | 378(62.1%) |
| Muslim | 112(18.4%) | |
| Protestant | 81(13.3%) | |
| Catholic | 38(6.2%) | |
| Caregivers’ Educational Status | Cannot read and write | 106(17.4%) |
| Elementary | 179(29.4%) | |
| High school | 157(25.8%) | |
| College Diploma | 98(16.1%) | |
| Degree and above | 69(11.3%) | |
| Caregivers’ Relationship with the Child | Mother | 474(77.8%) |
| Father | 51(8.4%) | |
| Grand Parent | 29(4.8%) | |
| Uncle Aunt | 49(8%) | |
| Other | 6(1%) | |
| Caregivers’ Ethnic Background | Amhara | 221(36.3%) |
| Oromo | 163(26.8%) | |
| Gurage | 122(20%) | |
| Tegaru | 97(15.9%) | |
| Others | 6(1%) | |
| Average Monthly Income of the Household | < 500ETB | 128(21%) |
| 500 -1000ETB | 82(13.5%) | |
| 1001 – 2000ETB | 228(37.4%) | |
| > 2000ETB | 171(28.1%) | |
Awareness about zinc and zinc source and zinc former usage
Pertaining to the exposure to message on zinc, 484 (79.5%) of the respondents heard about zinc. Health professionals were the major (63.6%) source of information about zinc, while radio/television/other posted materials also contributed. More than half (60.1%) of the respondents were aware that they can get zinc from health center, and private pharmacy was also mentioned by more than one fourth (27.6%) of the study participants as place where to get zinc. Zinc was used only by 35% of the study participants previously for diarrheal treatment. Of the 609 respondents, almost three-fourth (73.9%) of caregivers was willing to pay for zinc. There were participants (25.1%) who looked for charge free zinc (cost to pay ranging 0.00 - 2.5 $US). The median estimated cost of which participants were willing to pay for zinc was 6ETB [0.30 ±0.45 $US] (Table 2).
| Table 2: Zinc awareness, source, former usage and willingness to pay for (N = 609). | ||
| Variables | No (%) | |
| Have you ever heard about zinc? | Yes | 484(79.5) |
| No | 125(20.5) | |
| From where/How did you hear/see about Zinc? | Health professional | 308( 63.6) |
| Other | 176(36.4) | |
| Where can you find Zinc? | Health center | 366(60.1) |
| Hospital | 5(0.8) | |
| Private clinic | 19(3.1) | |
| Private pharmacy | 168(27.6) | |
| Don’t know | 51(8.3) | |
| Have you ever used zinc? | Yes | 215(35.3) |
| No | 394(64.7) | |
| Are you willing to pay for Zinc? | Yes | 301(73.9) |
| No | 111(25.1) | |
| Exchange rate in was 1 US$ for 20 ETB | ||
Zinc administration
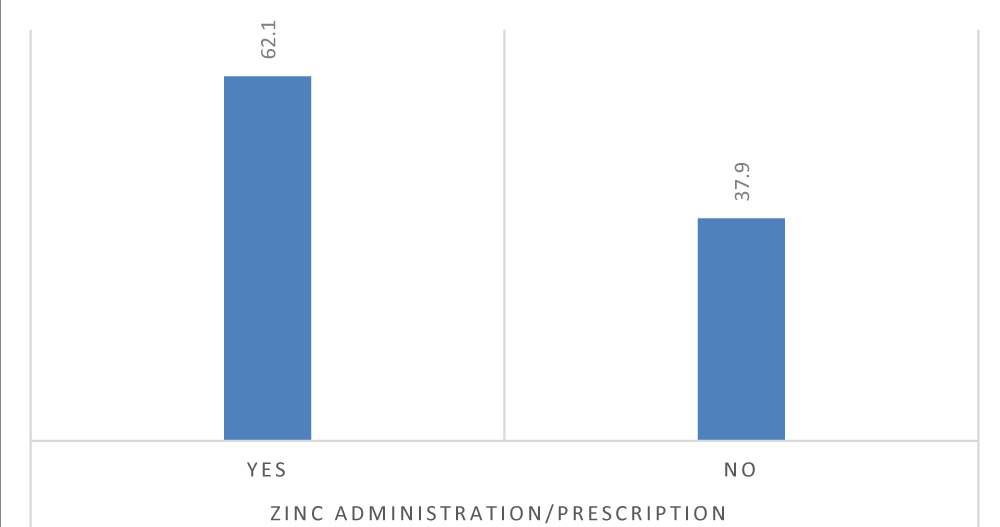
Zinc was not prescribed for more than one-third (37.9%) of children who attended health institutions because of diarrhea (Figure 1).
Figure 1: Percentage distribution of zinc prescription practice for children with diarrhea.
Out of the total zinc prescriptions, majority of zinc prescriptions (75.1%) were written by female health workers and professional nurses (52.9%). Almost one-fourth (24.6%) of the caretakers obtained zinc for free from the health centers they attended. Nearly all (93.8%) of the participants to whose child zinc was prescribed received counseling about diarrhea and zinc. In addition to zinc, ORS (64.69%), diarrheal syrup (31.5%) and antibiotics (3%) were prescribed to the children with diarrhea (Table 3).
| Table 3: Zinc prescription related information. | ||
| Variable | N (%) | |
| How did you obtain the zinc? | Free | 93(24.6) |
| Purchased | 285(75.4) | |
| Perceived charge of zinc | Not expensive | 130(34.4) |
| Affordable | 242(64) | |
| Expensive | 6 (1.6) | |
| Profession of the health worker who prescribed zinc | Health Officer | 122(32.3) |
| Professional Nurse | 200(52.9) | |
| Clinical Nurse | 49(13) | |
| General Practitioner | 7(1.9) | |
| Counseling on use of zinc? | Yes | 571(93.8) |
| No | 38(6.2) | |
| Sex of the health worker who prescribed zinc? | Male | 94(24.9) |
| Female | 284(75.1) | |
| ORS | 394(64.69) | |
| Other treatments given | Diarrheal Syrup | 192(31.5) |
| Antibiotics | 18(3) | |
| Others | 5(0.8) | |
Factors associated with zinc prescription
The multivariable logistic regression analysis showed that children with caretakers who had used zinc before were 2.3 times more likely to receive zinc prescription for diarrhea than their counter parts (AOR = 2.3; 95% CI: 1.34-4.01). Moreover, children whose caregivers had exposure to zinc related information were 2.6 times more likely to receive zinc prescription (AOR = 2.6; 95% CI: 1.53-4.60). This study also revealed that zinc was 6.9 times more likely (AOR = 6.9; 95%CI: 3.84-12.6) to be prescribed for children with diarrhea who were with caregiver willing to pay for zinc (Table 4).
| Table 4: Factors associated with zinc administration for children with diarrhea who attended health centers in Addis Ababa. | ||||
| Variable | Zinc Prescription | COR (95% CI) | AOR (95% CI) | |
| Yes | No | |||
| Education | ||||
| Cannot read and write | 69 | 38 | 1.00 | |
| Elementary | 71 | 107 | 1.4(0.85-2.3) | |
| High school | 68 | 89 | 1.5(0.9-2.4) | |
| College Diploma | 37 | 61 | 1.08(0.6-1.9) | |
| Degree and above | 17 | 52 | 0.35(0.16-0.75) | |
| Household income | ||||
| < 500 ETB | 91 | 37 | 1.00 | |
| 500-1000 ETB | 34 | 48 | 1.7(0.97-3.11) | |
| 10001-2000 ETB | 100 | 128 | 3.14(1.20- 4.50)** | |
| > 2000 | 60 | 111 | 1.3(0.8-2.1) | |
| seen/heard about zinc | ||||
| Yes | 182 | 302 | 0.93(0.62-1.3) | |
| No | 49 | 76 | 1.00 | |
| Where did you hear/see the message | ||||
| Health professional | 161 | 147 | 2.01(1.37-2.95)*** | 2.30(1.31-4.05)** |
| Other | 62 | 114 | ||
| Have you ever used | ||||
| Yes | 113 | 102 | 2.59(1.83-3.65)*** | 2.24(1.28-3.89)** |
| No | 118 | 276 | 1.00 | |
| Have you ever purchased | ||||
| Yes | 87 | 98 | 1.72(1.21-2.45)** | |
| No | 144 | 280 | 1.00 | |
| Willing to Pay for zinc | ||||
| Yes | 172 | 129 | 5.10(3.05-8.51)*** | 7.06(3.85-12.93)*** |
| No | 23 | 88 | 1.00 | |
| Counseling | ||||
| Yes | 215 | 356 | 0.83(0.42-1.61) | |
| No | 16 | 22 | 1.00 | |
| **p < 0.01; ***p < 0.001. | ||||
This study was conducted among pairs of caretakers and children with diarrhea to assess zinc prescription practice and identify associated factors in Addis Ababa, Ethiopia. Based on the finding of the current study, 62.1% of children received zinc prescription. Previous zinc usage, care givers exposure to zinc related messages, willingness to pay for zinc were variables associated with zinc prescription.
The proportion of children for whom zinc prescribed was 62.1%. The proportion was higher than figures from studies conducted in Nepal (15.4%) [22] and India (22%) [23]. But it was lower than the findings from study done in Kenya (64.30%) [24] and in Mali (66.6%) [25]. This may be due to previous zinc usage, exposure to message about the use of zinc as treatment for diarrhea, willingness to pay for zinc, socio economic variation and the type of health facilities the participants visited.
About 80% of the caretakers of children with diarrhea who participated in the current study heard about zinc that is serve as treatment for diarrhea. The result is higher than the findings of studies from Nepal (53%) [22], Uganda (17.2%) and Benin (72.1%) [26]. This may be due to the type of exposure to message on zinc treatment for diarrhea from health professionals and mass media.
Among all caretakers, 73.9% expressed their willingness to pay for zinc. The proportion is comparable to statistics from Nepal-70.5% [22] and Kenya-67% [27], but far lower than result from Bangladesh-92% [28].
Two-third (75.1%) of zinc prescription was written by female health care workers. Consistent to the finding of the current study, a research conducted in Nigeria also reported that much of the zinc prescriptions were by female health care workers (38.1%) [29]. With regard to health cadres with whom did the prescription were written, 65.8% were by Nurse, 32.3% by health officers and 1.9% general practitioners. In Kenya, 62.5% of the prescriptions were written by community health officers [27]. The difference might be due to the number dominancy of nurses in Ethiopian health care system and difference in health care system structure and cadre organization between the countries.
Children from caretakers exposed to messages about zinc from health care workers were 2.6 times (AOR = 2.6, 95% CI: 1.53-4.60) more likely to receive zinc prescription. The association is consistent with report of a study done in Kenya in which those who had recent contact with health care workers were reported for their higher chance receiving of zinc prescription. A study conducted in Nepal also strengthens the positive association between exposure to zinc related message and the chance of zinc prescription. It reported 2 times (AOR = 2.02, 95% CI: 1.85-2.19) more chance for those who were exposed to messages from media [22,30].
This study also revealed that children of caretakers who were willing to pay for zinc were seven times (AOR = 6.9; 95% CI: 3.84-12.6) more likely to receive zinc prescription than their counter parts. In agreement to the current finding, a study conducted in Kenya reported importance of caretakers willing for zinc usage as treatment of childhood diarrhea. In the Kenyan study caretakers in the zinc-user group were willing to pay more for a course of zinc in the future than non-user group [30].
Even though zinc prescription is recommended to be included in the integrated management of childhood illness for the management of diarrhea, in the study area it was not prescribed for considerable proportion of children with diarrhea. The proportion of caretakers who were not willing to pay for zinc and the need for charge free health service including zinc might have contributed for no zinc prescription. Previous experience in use of zinc for diarrheal management, exposure to zinc related message and willingness to pay for zinc were identified being positively associated with zinc prescription. Health care workers shall be encouraged to prescribe zinc to all children with diarrhea. Intervention to increase willingness to pay for zinc and zinc benefit communication shall be strengthened in parallel with operational researches
Ethics approval and consent to participate
Ethical clearance was obtained from ethical clearance committee of Debremarkos University. A written letter of requesting for cooperation was also handed to all of the included health centers. Oral consent was secured from each of the study participants. Their participation was on voluntary bases. Obscurity was assured throughout the data collection and management process.
Funding
Cost of data collection was covered by the authors.
Authors’ contribution
AW and MB: conception and design of the study; AW, MB and AKD: Data analysis, interpretation of results; AKD: manuscript drafting. AW and MB: Manuscript review. All authors read and approved the final manuscript.
The authors would like to acknowledge School of Public Health-Debre Markos University and study area administrative bodies for the assistances provided for the study. Study participants are also duly acknowledged for their valuable investment.
Availability of data and material
Important data already included in the manuscript.
Authors’ Information
AW Amref Health Africa, Addis Ababa, Ethiopia. MB: Charlotte, North Carolina Area, USA. AKD: School of Nursing, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia.
- World Health Organization (n.d.). Diarrhoea.https://www.who.int/topics/diarrhoea/en/
- World Health Organization. Diarrhoeal disease. 2017. https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease
- Robert EB, Saul SM, Jennifer B. Where and why are 10 million children dying every year? Lancet. 2003; 361; 2226–2334. PubMed: https://pubmed.ncbi.nlm.nih.gov/12842379/
- Liu L, Oza S, Hogan D, Chu Y, Perin J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016; 388: 3027–3035. PubMed: https://pubmed.ncbi.nlm.nih.gov/27839855/
- Roohani N, Hurrell R, Kelishadi R, Schulin R. Zinc and its importance for human health: An integrative review. J Res Med Sci. 2013; 18; 144–157. PubMed: https://pubmed.ncbi.nlm.nih.gov/23914218/
- Hannah Ritchie MR. (n.d.). Micronutrient Deficiency. https://ourworldindata.org/micronutrient-deficiency
- Solomons NW. Dietary sources of zinc and factors affecting its bioavailability. Food Nutr Bulletin. 2001; 22: 138–154.
- Federal Democratic Repulic of Ethiopia. The seqota declaration committed to ending stunting in children under two by 2030. 2019.
- Dafursa K, Gebremedhin S. Dietary Diversity among Children Aged 6-23 Months in Aleta Wondo District, Southern Ethiopia. J Nutr Metabol. 2019.
- Solomon D, Aderaw Z, Tegegne TK. Minimum dietary diversity and associated factors among children aged 6-23 months in Addis Ababa, Ethiopia. Int J Equity Health. 2017; 16: 181. PubMed: https://pubmed.ncbi.nlm.nih.gov/29025434/
- Temesgen H, Yeneabat T, Teshome M. Dietary diversity and associated factors among children aged 6–23 months in Sinan Woreda, Northwest Ethiopia: a cross-sectional study. BMC Nutr. 2018; 4: 1–8. PubMed: https://pubmed.ncbi.nlm.nih.gov/32153869/
- Gibson RS, Ferguson EL. Nutrition intervention strategies to combat zinc deficiency in developing countries. Nutr Res Rev. 1998; 11: 115–131. PubMed: https://pubmed.ncbi.nlm.nih.gov/19087462/
- Kabata A, Henry C, Moges D, Kebebu A, Whiting S, et al. Determinants and Constraints of Pulse Production and Consumption among Farming Households of Ethiopia. J Food Res. 2016; 6: 41.
- Hailu A, Henry C, Kebebu A, Whiting S. Effectiveness of the women’s development team leaders in delivering nutrition education on pulse sprouting in Southern Ethiopia. African J Food, Agri Nutrit Develop. 2020; 20: 15331–15343.
- Yetnayet M, Henry CJ, Berhanu G, Whiting SJ, Regassa N. Nutrition education promoted consumption of pulse based foods among rural women of reproductive age in Sidama zone, Southern Ethiopia. African J Food, Agri Nutrit Develop. 2017; 17: 12377–12394
- Gibson RS, Abebe Y, Hambidge KM, Arbide I, Teshome A, et al. Inadequate feeding practices and impaired growth among children from subsistence farming households in Sidama, Southern Ethiopia. Matern Child Nutr. 2019; 5: 260–275. PubMed: https://pubmed.ncbi.nlm.nih.gov/20572929/
- Sharma K, Mogensen KM, Robinson MK. Pathophysiology of Critical Illness and Role of Nutrition. Nutr Clin Pract. 2019; 34: 12–22. PubMed: https://pubmed.ncbi.nlm.nih.gov/30580456/
- Hambidge KM. Zinc and diarrhea. Acta Paediatr Suppl. 1992: 81: 82–86. PubMed: https://pubmed.ncbi.nlm.nih.gov/1421947/
- World Health Organization and United Nations Children Fund. Clinical management of acute diarrhoea acute diarrhoea. 2004.
- Federal Democratic Republic of Ethiopia. Summary and Statistical Report of the 2007 Population and Housing Census:Population Size by Age and Sex. Addis Ababa.2008.
- Lemeshow S Jr, D. W. H, Klar, J, Lwanga SK. Adequacy of Sample Size in Health Studies. Biometrics. 1991; 47: 347.
- Wang W, Vicki M. Introducing zinc through the private sector in Nepal for the treatment of childhood diarrhea. 2009.
- Pathak D, Pathak A, Marrone G, Diwan V, Lundborg CS. Adherence to treatment guidelines for acute diarrhoea in children up to 12 years in Ujjain, India - A cross-sectional prescription analysis. BMC Infectious Diseases.2011; 11: 32.
- Jamlick K. Zinc prescription in children with diarrhoea admitted to 22 Kenyan hospitals. Global Epidemiology in a Changing Environment: The Circumpolar Perspective. Ancholaske, Alaska USA. 2014.
- Winch PJ, Gilroy KE, Doumbia S, Patterson AE, Daou Z, et al. Short report: Prescription and administration of a 14-day regimen of zinc treatment for childhood diarrhea in Mali. Am J Trop Med Hyg. 2006 74: 880–883. PubMed: https://pubmed.ncbi.nlm.nih.gov/16687696/
- Macdonald V, Sanders E. Marketing Zinc for Childhood Diarrhea Treatment: Results from household and provider surveys in Benin and Uganda. 2012.
- Jamlick K. Zinc prescription in children with diarrhoea admitted to 22 Kenyan hospitals. Global Epidemiology in Chnging Environment: The Circumpolar Perspective, 2014.
- Akhter S, Larson CP. Willingness to pay for zinc treatment of childhood diarrhoea in a rural population of Bangladesh. Health Policy Plan. 2010; 25: 230–236. PubMed: https://pubmed.ncbi.nlm.nih.gov/19955094/
- Omuemu VO, Ofuani IJ, Kubeyinje IC. Knowledge and use of zinc supplementation in the management of childhood diarrhoea among health care workers in public primary health facilities in Benin-City, Nigeria. Glob J Health Sci. 2012; 4: 68–76. PubMed: https://pubmed.ncbi.nlm.nih.gov/22980153/
- Otieno GA, Bigogo GM, Nyawanda BO, Aboud F, Breiman RF, et al. Caretakers’ perception towards using zinc to treat childhood diarrhoea in rural Western Kenya. J Health Popul Nutr. 2013; 31: 321–329. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3805881/