More Information
Submitted: October 17, 2022 | Approved: November 24, 2022 | Published: November 25, 2022
How to cite this article: Balta B, Fanta A. Survival and predictors of mortality among HIV-infected adults receiving ART in Hawassa comprehensive specialized hospital, Sidama regional state, Ethiopia. J Adv Pediatr Child Health. 2022; 5: 042-049.
DOI: 10.29328/journal.japch.1001052
Copyright License: © 2022 Balta B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Antiretroviral therapy; Human immunodeficiency virus; Mortality; Survival; Ethiopia
Survival and predictors of mortality among HIV-infected adults receiving ART in Hawassa comprehensive specialized hospital, Sidama regional state, Ethiopia
Bargude Balta1* and Amanuel Fanta2
1Comprehensive Specialized Hospital, College of Health Sciences, Hawassa University, Ethiopia 2Hawassa College of Health Sciences, Department of Nursing, Hawassa, Ethiopia
*Address for Correspondence: Bargude Balta, Comprehensive Specialized Hospital, College of Health Sciences, Hawassa University, Ethiopia, Email: [email protected]
Background: Having claimed lives, HIV/AIDS is still a significant global public health concern. Antiretroviral therapy (ART) is now widely available, and this rapid expansion of access is dramatically improving HIV epidemic survival rates worldwide.
Objectives: The aim of this study was to identify the mortality risk factors and survival status of ART patients attending Hawassa Comprehensive Specialized Hospital in 2020.
Methods: In a five-year retrospective cohort research, all patients seen between January 2015 and December 2019 were analyzed. The data were analyzed with SPSS 25.0. The Kaplan-Meier Log-rank model was employed to gauge the survival time of ART patients based on explanatory variables. Both bivariate and multivariate Cox proportional hazards regression models were employed to identify the independent causes of mortality.
Results: Patients on ART had a 74% overall survival probability. With a median survival of 34 months, there are 0.135 deaths for every 100 person-years. Hemoglobin level (HR = 2.38; 95% CI = 3.3-6.3), WHO clinical stage III and IV (HR = 3; 95% CI = 2.2-9.5, p = 0.04), Age > = 60 (HR = 1.6; 95% CI = 1.3-2, p = 0.04) and Functional status bed ridden (HR = 3.1; 95% CI = 1.2-9.4, p = 0.04) were all independent predictors of death among RVI patients.
Conclusion: In comparison to trials conducted in wealthy countries, the survival rate of ART patients in this study was low. Patients who are anemic; WHO advanced clinical stage; old age, and functional status bedridden should be closely followed and monitored.
Having taken approximately 33 million lives to date, HIV/AIDS continues to be a significant global public health burden. Despite this, HIV infection has developed into a manageable chronic health disease that enables individuals living with HIV to live long and healthy lives thanks to increasing access to effective HIV prevention, diagnosis, treatment, and care, including opportunistic infections. An estimated 38.0 million people were predicted to be HIV-positive as of the end of 2019 [1,2]. In 2019, the main population groups and their sexual partners were responsible for more than 60% (about 62%) of all new HIV infections worldwide among people aged 15 to 49.
These groups were responsible for more than 95% of new HIV infections in each of these regions, including Eastern Europe and Central Asia, Asia and the Pacific, Western and Central Europe and North America, and the Middle East and North Africa. The WHO African Region is home to 25.7 million HIV-positive individuals or more than two-thirds of the global total [1,3,4]. Ethiopia is one of the countries in Sub-Saharan Africa that has been most severely affected by the HIV pandemic. The number of HIV-positive Ethiopians is thought to be 738,976. [5]. According to the Ethiopian Demographic and Health Survey 2016, the overall HIV prevalence is 0.9% and the urban prevalence is 2.9%, which is seven times higher than the rural prevalence (0.4%) (EDHS 2016).
The World Health Organization guidelines, which recommend early ART for all PLHIV, regardless of CD4 cell count, were based on a growing body of evidence demonstrating the increased risk of AIDS or death associated with delaying treatment, according to the 2016 EDHS reports that HIV incidence varies by area, ranging from less prevalent in [6]. Antiretroviral therapy (ART) availability is being quickly expanded, which is dramatically enhancing worldwide HIV epidemic survival and reducing AIDS-related mortality rates. Increased ART use has, to date, largely in developing and underdeveloped nations decreased the estimated 6.6 million AIDS-related deaths that occurred globally [3,7]. Service coverage has continuously risen as a result of concerted international efforts to prevent HIV. In 2019, 68% of adults with HIV around the globe were taking antiretroviral medications for the rest of their lives (ART).
Antiretroviral therapy (ART) enhances immune system performance while reducing HIV replication and new cell infection. ARV medication consequently enhances the survival and quality of life of HIV carriers [1,8]. In Ethiopia, antiretroviral treatment (ART) was first made available in 2005. Only 426,000 of the projected 738,976 HIV-positive Ethiopians who need antiretroviral medication (ART) are now receiving it [5,9].
A few studies on the mortality of HIV adults completed in Ethiopia and other nations demonstrate that prompt ART introduction among HIV/AIDS adults lowers mortality and has a favorable effect on survival for those particular study groups. Additionally, cotrimoxazole prophylaxis therapy (CPT), older age, male sex, baseline hemoglobin, CD4 count, WHO clinical stage and HAART use.
Study setting and period
The research was done at the ART and IPT services offering Hawassa University Specialized Hospital. It is 273 kilometers south of Addis Ababa. A teaching hospital with basic facilities for HIV care and treatment, with an established clinical set-up and highly skilled medical staff, the hospital provides services for about two million individuals. Since July 2006, the hospital has been providing pre-ART and ART services.
Study design
An Institutional based retrospective study was conducted between January 2015 to December 2019 in Hawassa comprehensive specialized hospital to assess survival in PLWHA and those who are on ART.
Population
Source population: A person living with HIV/AIDS, age ≥ 15 years and started ART treatment in Hawassa comprehensive specialized hospital.
Study population: Those patients fulfilling the following criteria.
Inclusion criteria
Positive adults aged 15 yrs or older who started ART
HIV patients with the complete intake form, registers and follow-up form
Exclusion criteria
Diagnosis is made outside of health institution
Women who were pregnant at the time of ART initiation and lactating mother.
Sample size determination
The sample size was determined using double population proportion formula by considering CD4, functional status and WHO stage as the major predictor variables{Formatting Citation}. Moreover, CD4 is considered an independent predictor since it gives the maximum sample size. The sample size was calculated by using open Epi info version 7 statistical packages.
P1: is the percent of completed with the outcome
P2: is the percent of non-completers. With the outcome
Z α/2: is taking CI 95%: 80% power
r: is the ratio of non-completers to completers1:1.
Sample size calculation was done by considering determinant
| S.N | Variables | CI | Assumptions | Total sample size | Reference |
| 1. | CD4 | 95% | P1=54% P2=7.5% |
483 | [10] |
| 2. | WHO stage | 95% | P1=65% P2=34% |
92 | [11] |
| 3. | Bedridden functional status |
95% | P1=66% P2=33% |
88 | [12] |
P1: is the percent of completed with the outcome |
Z α/2: is taking CI 95% |
• r is the ratio of non-completers to completers 1:1
Then the largest sample size (n = 483)
Sampling technique
Study participants were selected by using a systematic random sampling method using commands in Excel all 464 records of patients receiving ART in Hawassa comprehensive specialized hospital were listed in an excel spreadsheet, and a randomly selected 483 patients were studied.
Dependent and Independent variables
Time to the event in a month served as the primary outcome metric. The interval between the start of ART treatment and the event or censoring date was used to compute the time of survival in months. Socio-demographic traits and baseline clinical data were the independent determining variables. The ART patients were monitored up until the time of death, loss to follow-up, transfer out, or study conclusion. If a patient was lost for follow-up or transferred out, they were regarded as censored.
Data collection procedure and quality control
A form for gathering data was created using the ART clinic’s entry and follow-up procedures. Reviewing the pre-ART register, laboratory request, and follow-up form allowed for the collection of the data. Prior to beginning ART, the most recent test findings served as the baseline value. By creating the necessary data collection tools and maintaining close supervision, data quality was managed. The accuracy of each filled-out data collection form was verified.
Entry and analysis
The data was cleaned and coded before being entered into Epidata 4.6.2. An analysis based on a 5 - year cohort follow-up was conducted. Finally, data was exported for processing into SPSS version 25.0. Interquartile range (IQR) was used in the presentation of descriptive statistics for numeric variables, whereas frequency and percentages were used for categorical variables. By using the Kaplan-Meier Log-rank model to calculate the TB Occurrence time based on explanatory variables, the TB-free survival time was calculated. To the independent determinants, bivariate and multivariate Cox proportional hazards regression models were run.
Operational definition
Lost to follow-up: If a patient discontinued ART for one to three months as recorded by the ART physician
Event: - PLWHIV on ART, who died during the study period
Survival: lack of experience with death.
Ethical considerations
Ethics approval and consent to participate: The research and ethics commission (REC) of Addis Abeba University’s School of Nursing and Midwifery’s College of Health Sciences granted its approval. The hospital’s outpatient administrators provided a letter of authorization to view patient data. Since we are reporting on a retrospective analysis of medical records, the ethics committee waived the requirement for informed consent and completely anonymized all data before we had access to it.
483 people in all were surveyed and 262 (54.2%) of them were men. The age range of the respondents was 18 to 68 years, with a mean age of 32.8 and 12.8 years (Mean SD). 56.1% of the 271 respondents, or more than half, were married. Regarding participant education, 271 (56.1%) of the respondents had secondary education or higher, while the remaining 212 (43.9%) had only primary education. Only 26 people, or 25.50% of the population, went to college. 51.1% of the 247 respondents, or nearly half, have used drugs or alcohol in the past.
By profession, 123 respondents (25.5%) worked in the government. Only 186 participants, or 38.5%, came from rural areas, with urban participants making up the majority. Regarding religion, 225 people (46.6%) identified as Orthodox believers (Table 1).
| Table 1: Socio–demographic characteristics of HIV patients who were enrolled for ART care at Hawassa University Comprehensive Specialized Hospital Sidama, Ethiopia, from January 2015 to December 2020 (n = 483). | |||
| Characteristics | Status at last contact Death Censored |
Total | |
| Age in years [mean = 32.8, SD = 12.8] |
|||
| 18 – 39 | 8(2.5%) | 313(97.5%) | 321(66.5%) |
| 40 – 59 | 5(3.5%) | 138(96.5%) | 143(29.6%) |
| > = 60 | 13(68.4%) | 6(31.6%) | 19(3.9%) |
| Sex | |||
| Male | 10(4.5%) | 211(95.5%) | 221(45.8%) |
| Female | 16(6.1%) | 246(93.9%) | 262(54.2%) |
| Marital Status | |||
| Never Married | 4(3.7%) | 103(96.3%) | 107(22.2%) |
| Married | 15(5.5%) | 256(94.5%) | 271(56.1%) |
| Separated | 3(8.6%) | 32(94.1%) | 35(7.2%) |
| Widowed | 1(4.8%) | 20(95.2%) | 21(4.3%) |
| Divorced | 3(6.1%) | 46(93.9%) | 49(10.1%) |
| Residence | |||
| Urban | 15(5.1%) | 282(94.9%) | 297(61.5%) |
| Rural | 11(5.9%) | 175(94.1%) | 186(38.5%) |
| Religion | |||
| Protestant | 10(5.9%) | 159(34.8%) | 169(35%) |
| Orthodox | 12(5.3%) | 213(94.7%) | 225(46.6%) |
| Muslim | 3(5.8%) | 49(94.2%) | 52(10.8%) |
| Catholic | 1(3.8%) | 25(96.2%) | 26(5.4%) |
| Other | 0 | 11(100%) | 11(2.3%) |
| Substance Use | |||
| Yes | 16(6.5%) | 231(93.5%) | 247(51.1%) |
| No | 10(4.2%) | 226(95.8%) | 236(48.9%) |
| Educational Status | |||
| No education | 5(8.1%) | 57(91.9%) | 62(12.8%) |
| Primary | 12(8%) | 138(92%) | 150(31.1%) |
| Secondary | 6(3.4%) | 171(96.6%) | 177(36.6%) |
| More than Secondary | 3(3.2%) | 91(96.8%) | 94(19.5%) |
| Occupation | |||
| Farmer | 10(17.5%) | 47(82.5%) | 57(11.8%) |
| Merchant/Trader | 3(2.7%) | 108(97.3%) | 111(23%) |
| Government Employed | 2(1.6%) | 121(98.4%) | 123(25.5%) |
| Non – Government | 3(7.1%) | 39(92.9%) | 42(8.7%) |
| Day Laborer | 1(2.3%) | 43(97.7%) | 44(9.1%) |
| Jobless | 2(6.3%) | 30(93.8%) | 32(6.6%) |
| Driver | 2(5.1%) | 37(94.9%) | 39(8.1%) |
| Retired/housewives/Student (other) | 3(8.8%) | 32(91.4%) | 34(7%) |
More than half 356 (73.7%) of the study participants were WHO clinical Stage I/II and medium of current CD4 count = 456 cells/µL. Seventy-six (76.2%) of respondents were in CPT prophylaxis and (93.8%) were IPT completed. Three hundred six (69.7%) of respondents’ functional status was working and more than half of respondents’ BMI were less than 18 kg/m2 (Table 2).
| Table 2: Clinical characteristics of HIV patients who were enrolled for IPT care at Hawassa University Comprehensive Specialized Hospital, Sidama, Ethiopia from January 2015 to December 2020 (n = 483). | |||
| Characteristics | Status at last contact Death Censored |
Total | |
| WHO clinical Stage | 1 | ||
| I and II | 6(1.7%) | 350(98.3%) | 356(73.7%) |
| III and IV | 20(15.7%) | 107(84.3%) | 127(26.3%) |
| CD4 cell count (Cells/µL) | |||
| < = 200 | 12(17.4%) | 57(82.6%) | 69(14.3%) |
| > 200 | 14(3.4%) | 400(96.6%) | 414(85.7%) |
| Medium of current CD4 count = 456 cells/µL, (IQR, 314 – 661) and 231 cells/ µL (IQR, 105 – 400) | |||
| BMI | |||
| < 18 kg/m2 | 19(7.1%) | 248(92.9%) | 267(55.3%) |
| > 18 kg/m2 | 7(3.2%) | 209(96.8%) | 216(44.7%) |
| Medium BMI = 20.29 kg/m2 (IQR, 18.49 – 22.36) |
|||
| CPT use | |||
| Yes | 18(4.9%) | 350(95.1%) | 368(76.2%) |
| No | 8(7.0%) | 107(93%) | 115(23.8%) |
| IPT use | |||
| Yes | 23(5.1%) | 430(94.9%) | 453(93.8%) |
| No | 3(10.0% | 27(90%) | 30(6.2%) |
| HIV/TB co – infection | |||
| Yes | 7(13.5%) | 45(86.5%) | 52(10.8%) |
| No | 19(4.4%) | 4106(95.6%) | 429(89.2%) |
| Chronic illness | |||
| Yes | 11(47.8%) | 12(52.2%) | 23(4.8%) |
| No | |||
| Hemoglobin | |||
| > = 11 mg/dl(Normal) | 16(4.1%) | 374(95.9%) | 390(80.7%) |
| < 11 mg/dl(Anemia) | 10(10.8%) | 83(89.2%) | 93(19.3%) |
| Functional status | |||
| Working | 3(0.9%) | 333(99.1%) | 336(69.7%) |
| Ambulatory | 7(6.9%) | 99(93.4%) | 106(22%) |
| Bed ridden | 16(40%) | 24(60%) | 40(8.3%) |
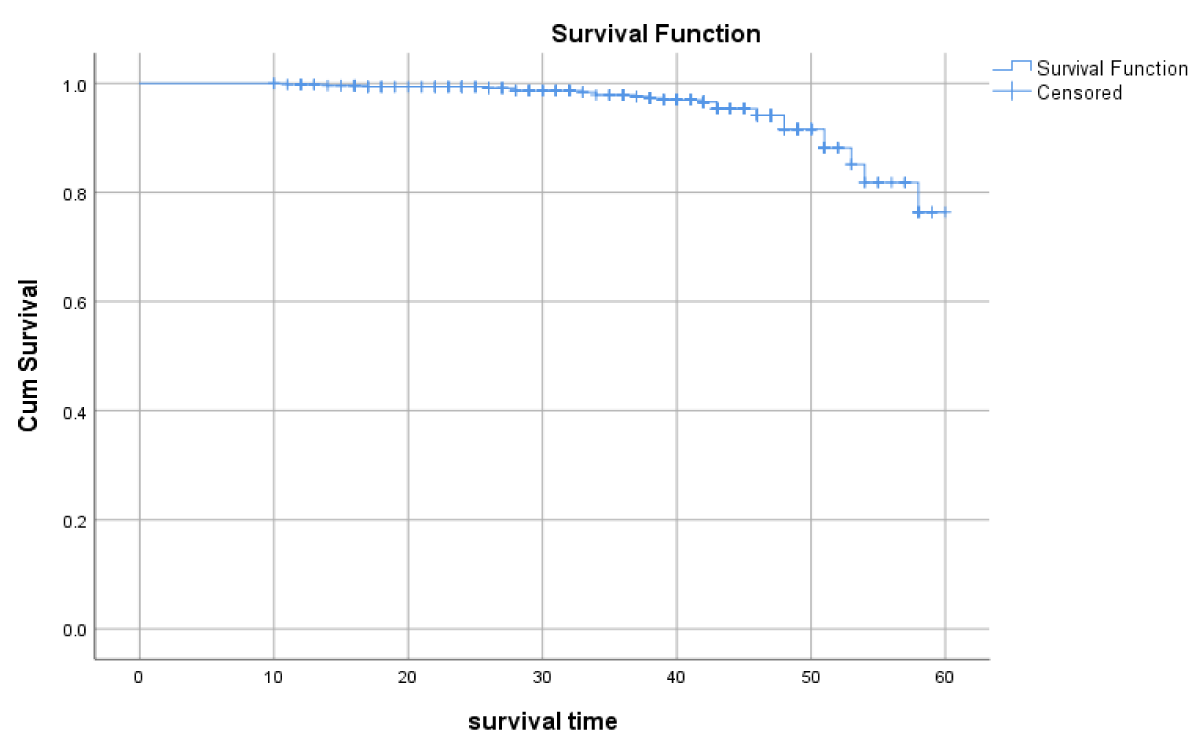
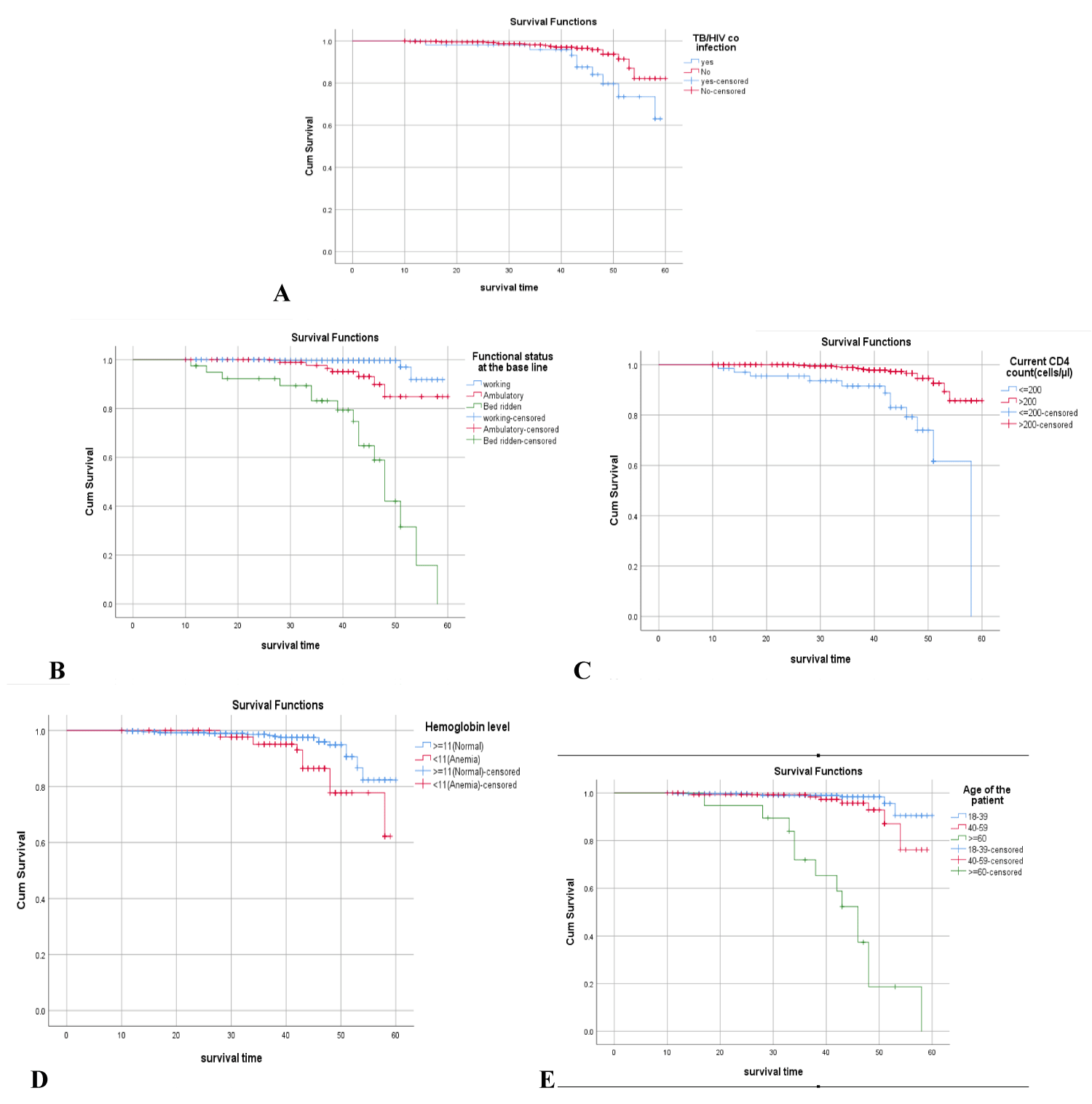
Survival experience among different groups of ART patients in log-rank test 26 patients (5.4%) died during the follow-up period, with a death incidence rate of 0.135 per 100 person-years. The survival probability at the eleventh month of ART initiation was 99.8%. This proportion reduces to 99.6, in the 14th month and is preceded by 99.4%, 97.9%, 91.6%, and 76.4% in the second, third, fourth, and the end of the follow-up period, respectively (Figure 1). Baseline WHO clinical stages (Log-rank, p ≤ 0.01), functional status (Log-rank, p ≤ 0.001), age (Log-rank, p ≤ 0.001base line hemoglobin (Log-rank, p ≤ 0.001), and CD4 count (Log-rank, p ≤ 0.01) were variables that showed the significant association with the survival of patients on ART within Log-rank test (Figure 2) (Table 3).
Figure 1: Shows the overall survival probability of patients on ART starting from the initiation of ART until the end of the study period among PLWHA, Hawassa town, Southern Ethiopia, November 2020.
Figure 2: Kaplan-Meier survival curves show for comparison of (A) TB/HIV co-infection,(Log-rank test; p ≤ 0.01); (B) Functional status, (Log-rank test; p ≤ 0.01) (C) CD4 Cell count status, (Log-rank test, p ≤ 0.01); (D) Hemoglobin count, (Log-rank test; p ≤ 0.01) and (E) Age of the patients, (Log-rank test; p ≤ 0.01) at baseline among PLWHA, Hawassa town, Southern Ethiopia, November 2020.
| Table 3: Baseline characteristics and probability of ART survival during 5 years of follow–up (Kaplan–Meier method) of HIV patients receiving ART, Hawassa University, Comprehensive Specialized Hospital, Sidama, Ethiopia from January 2015 to December 2019. (n = 483). | |||
| Characteristics (Variables) |
Mean survival time/Probability in month over 5 yr (95% CI) |
Log rank test | p – value |
| Age in years [mean = 32.8,SD = 12.8] |
|||
| 18 – 39 | 58.89(57.95,59.85) | 141 | p ≤ 0.001 |
| 40 – 59 | 56.68(55.01,58.36) | ||
| > = 60 | 42.99(37.68,48.31) | ||
| WHO clinical stage | 40 | p ≤ 0.01 | |
| I & II | 58.97(58.11,59.84) | ||
| III & IV | 51.61(49.50,53.72) | ||
| CD4 cell count (Cells/µL) | 51.81(48.41,55.22) | 29.5 | p ≤ 0.001 |
| < = 200 | 54.95(52.32, 57.59) | ||
| > 200 | 39.85(35.43, 44.26) | ||
| Functional status | |||
| Working | 58.37(57.62, 59.11) | 120 | p ≤ 0.001 |
| Ambulatory | 57.34(55.43,59.26) | ||
| Bed ridden | 55.52(41.14,49.91) | ||
| HIV/TB co – infection | |||
| Yes | 54.69(52.01, 57.38) | 6.10 | p ≤ 0.01 |
| No | 57.88(56.79,58.97) | ||
| Hemoglobin | |||
| > = 11 g/dl(Normal) | 57.94(56.86,59.01) | 8.32 | p ≤ 0.01 |
| <11 g/dl(Anemia) | 55.11(52.99,57.23) | ||
Modeling of risk factors that are effective in the survival rate of patients on ART by using the Cox regression model.
To identify the independent predictors of survival after initiation of ART, Bivariate and multivariate Cox regression models were used. Bivariate Cox regression model, baseline WHO clinical stage, CD4, age, hemoglobin and functional status and HIV/TB co-infection showed significant association with early mortality after initiation of ART (Table 2). After multivariate analysis, four baseline factors could be independently identified: hemoglobin level (HR = 2.38;95% CI = 3.3-6.3); WHO clinical stage III and IV (HR = 3; 95% CI = 2.2-9.5, p = 0.04); Age > = 60 (HR = 1.6; 95% CI = 1.3–2, p = 0.04); Functional status bed ridden (HR = 3.1; 95% CI = 1.2-9.4, p = 0.04); were independent predictors of mortality among RVI patients (Table 4).
| Table 4: Cox regression analysis of the determinants of the incidence of TB among adults, who completed IPT care at Hawassa university comprehensive specialized hospital in Sidama Regional State, January 2015 to December 2019 (n = 483). | ||||
| Characteristics (Variables) | CHR (95% CI) | p – value | AHR (95% CI) | p – value |
| Age in years [mean = 32.8, SD = 12.8] | ||||
| 18 – 39 | 1.00(Ref) | 1.00(Ref) | ||
| 40 – 59 | 0.03(0.11 – 0.074) | p ≤ 0.01 | 0.11(0.03 – 0.4) | 0.061 |
| > = 60 | 2.3(0.3 – 15) | p ≤ 0.01 | 1.6(1.3 – 2) | 0.04 |
| WHO clinical stage | ||||
| I &II | 1.00(Ref) | p ≤ 0.01 | 1.00(Ref) | p ≤ 0.01 |
| III&IV | 3(2.2 – 9.5) | |||
| 10.75(4.3 – 26.8) | ||||
| CD4 cell count (Cells/µL) | ||||
| < = 200 | 1.00(Ref) | p ≤ 0.01 | 0.59 (0.15 – .2.26) | 0.44 |
| > 200 | 0.15(0.07 – 0.33) | p ≤ 0.01 | 1.00 Ref) | |
| Functional status | ||||
| Working | 1.00(Ref) | p ≤ 0.01 | 1.00 (Ref) | |
| Ambulatory | 0.01(0.005 – 0.065) | p ≤ 0.01 | 0.05(0.01 – 0.23) | p ≤ 0.01 |
| Bed ridden | 1.4(1 – 3.5) | p ≤ 0.01 | 3.1(1.2 – 9.4) | p ≤ 0.01 |
| HIV/TB co – infection | ||||
| Yes | 2.73(1.19 – 6.26) | 0.02 | 0.96(0.35 – 2.6) | 0.93 |
| No | 1.00(Ref) | p ≤ 0.01 | 1.00 Ref) | |
| Hemoglobin > = 11 g/dl(Normal) | 1.00(Ref) | p ≤ 0.01 | 1.00(Ref) | |
| <11 g/dl(Anemia) | 3.34(0.15 – 0.73) | 0.26 | 2.38(3.3 – 6.3) | p ≤ 0.01 |
In this retrospective cohort analysis, we found that CD4 cell count = 200 (Cells/L), advanced WHO staging (III and IV) and hemoglobin functional status were significant independent predictors of decreased survival in patients with HIV/AIDS following ART commencement. In univariate analysis, clinical AIDS stage at treatment initiation, baseline CD4 count, hemoglobin, age, HIV/TB co-infection and functional status were all substantially related to patient survival on ART. In a multivariate analysis, the only variables still significantly linked with survival were hemoglobin 11 g/dl (Anemia), WHO clinical stage, and functional level.
In 19194 PYO, there were 26 fatalities (5.4%) in our study, at a rate of 0.135 per 100 PYO. The cohort’s estimated survival probability at 1 - 5 years was, respectively, 99.8%, 99.4%, 97.9%, 91.6% and 76.4%. Comparing this finding to other research in Africa shows that ART patients had a greater survival rate. The likelihood of remaining alive on ART at 6, 12 and 18 months, respectively, was 89.8%, 83.4% and 78.8%, according to the same study [13]. However, especially in the first six months, the mortality rate was equivalent to those of the majority of studies [12,14,15]. This may be explained by the fact that the majority of the study’s participants had advanced diseases.
After correcting for confounding variables, our data corroborate the association between WHO staging (III and IV) and death, which is consistent with studies conducted in the north and west Ethiopia, which reveal comparable results of high mortality among advanced WHO clinical stage and correspondingly [2,6,8]. Another study, done in south Ethiopia and the Debremarkos referral hospitals, discovered that patients with WHO stages II and IV at the start of the study had a higher risk of death than people with WHO stages I and II who were mobile or bedridden. A five-year retrospective cohort research in Tanzania’s Kagera Region produced similar findings as the prior study [16].
A study conducted in Cameroon’s Far-North Province revealed that individuals with low hemoglobin levels upon diagnosis had nearly twice the chance of death as patients with high hemoglobin levels 2.38. (3.3 - 6.28). (0.0478) [17].
Our study results also suggest a similar trajectory, which could be attributed to hematologic difficulties, with patients progressing to AIDS at a faster rate and patients with hemoglobin levels less than 11 g/dl (Anemia) having a greater mortality rate in response to the viral killing. A South African study discovered that a decreased hemoglobin content of 8 g/dl was one of the key indications of higher mortality in HIV/AIDS patients. [18]. This outcome is identical to the current study. Similarly, a meta-analysis research in Adults Starting Antiretroviral Therapy (ART) in Low- and Middle-Income Countries.
In this study, the patient’s functional status was used to determine their survival status. The patients’ bedridden and ambulatory status was found as the key deciding factor. This is similar to the studies done in the Somali region with the result of a bedridden functional status. Other African researchers have found that functional level, particularly bedridden and ambulatory status, is a predictor of ART patient survival [8,19-23].
A comparable study conducted in the Far East and India reveals that the functional condition of ART patients was a major factor in mortality and survival over the study period [24-29].
We are quite appreciative of the Hawassa University Comprehensive Specialized Hospital and its College of Health Sciences. We also acknowledge the study participants, data collectors and staff of the ART clinic at Hawassa University’s Hawassa Comprehensive Specialized Hospital. A preprint has already been released.
Availability of data and materials
The corresponding author will provide the datasets used in the current work upon reasonable request from individuals who are interested.
Ethics approval and consent to participate
The Research and Ethics Commission (REC) of Addis Ababa University’s School of Nursing and Midwifery, College of Health Sciences, granted ethical approval. The hospital outpatient administration of Hawassa University specialized hospital granted permission to examine patients’ data. Because we are reporting on a retrospective analysis of medical records, all data were fully anonymized before we obtained them and the ethics committee waived the informed consent requirement.
Funding
The research was funded by Addis Ababa University. The University does not have any role in the design of the study and data collection, analysis and interpretation of data and in writing the manuscript should be declared.
Limitations
Due to Incomplete records being eliminated from the data, it affected the strength of associations, so the death rate could be underestimated or overestimated. The study was retrospective, and there was a risk of bias due to uncertainty on previous data.
Authors’ contribution
BB, and AF, conceived, designed and developed the data collection instruments. BB and AF performed the statistical analysis and wrote all versions of the manuscript. All authors critically revised and approved the final manuscript.
- WHO fact sheet 2019. HIV/AIDS . HIV/AIDS. 2020. https://www.who.int/news-room/fact-sheets/detail/hiv-aids
- Poorolajal J, Hooshmand E, Mahjub H, Esmailnasab N, Jenabi E. Survival rate of AIDS disease and mortality in HIV-infected patients: a meta-analysis. Public Health. 2016;139:3-12. http://dx.doi.org/10.1016/j.puhe.2016.05.004
- Misgina KH, Weldu MG, Gebremariam TH, Weledehaweria NB, Alema HB, Gebregiorgis YS, Tilahun YG. Predictors of mortality among adult people living with HIV/AIDS on antiretroviral therapy at Suhul Hospital, Tigrai, Northern Ethiopia: a retrospective follow-up study. J Health Popul Nutr. 2019 Nov 29;38(1):37. doi: 10.1186/s41043-019-0194-0. PMID: 31783924; PMCID: PMC6883545.
- Dawood H, Hassan-Moosa R, Zuma NY, Naidoo K. Mortality and treatment response amongst HIV-infected patients 50 years and older accessing antiretroviral services in South Africa. BMC Infect Dis. 2018 Apr 10;18(1):168. doi: 10.1186/s12879-018-3083-z. PMID: 29636023; PMCID: PMC5894176.
- EFMOH: Ministry of Health Federal Democratic Republic of Ethiopia. National Guidelunes for comprehensive HIV Prevention, Care and Treatment. 2017;44–6.
- Mangal TD, Meireles MV, Pascom ARP, de Almeida Coelho R, Benzaken AS, Hallett TB. Determinants of survival of people living with HIV/AIDS on antiretroviral therapy in Brazil 2006-2015. BMC Infect Dis. 2019 Feb 28;19(1):206. doi: 10.1186/s12879-019-3844-3. PMID: 30819120; PMCID: PMC6396460.
- Onyango DO, Yuen CM, Cain KP, Ngari F, Masini EO, Borgdorff MW. Reduction of HIV-associated excess mortality by antiretroviral treatment among tuberculosis patients in Kenya. PLoS One. 2017 Nov 16;12(11):e0188235. doi: 10.1371/journal.pone.0188235. PMID: 29145454; PMCID: PMC5690617.
- Seyoum D, Degryse JM, Kifle YG, Taye A, Tadesse M, Birlie B, Banbeta A, Rosas-Aguirre A, Duchateau L, Speybroeck N. Risk Factors for Mortality among Adult HIV/AIDS Patients Following Antiretroviral Therapy in Southwestern Ethiopia: An Assessment through Survival Models. Int J Environ Res Public Health. 2017 Mar 12;14(3):296. doi: 10.3390/ijerph14030296. PMID: 28287498; PMCID: PMC5369132.
- Assebe LF, Reda HL, Wubeneh AD, Lerebo WT, Lambert SM. The effect of isoniazid preventive therapy on incidence of tuberculosis among HIV-infected clients under pre-ART care, Jimma, Ethiopia: a retrospective cohort study. BMC Public Health. 2015 Apr 10;15:346. doi: 10.1186/s12889-015-1719-0. PMID: 25886730; PMCID: PMC4394593.
- Tiruneh G, Getahun A, Adeba E. Assessing the Impact of Isoniazid Preventive Therapy (IPT) on Tuberculosis Incidence and Predictors of Tuberculosis among Adult Patients Enrolled on ART in Nekemte Town, Western Ethiopia: A Retrospective Cohort Study. Interdiscip Perspect Infect Dis. 2019 May 2;2019:1413427. doi: 10.1155/2019/1413427. PMID: 31186628; PMCID: PMC6521313.
- Yiannoutsos CT, Johnson LF, Boulle A, Musick BS, Gsponer T, Balestre E, Law M, Shepherd BE, Egger M; International Epidemiologic Databases to Evaluate AIDS (IeDEA) Collaboration. Estimated mortality of adult HIV-infected patients starting treatment with combination antiretroviral therapy. Sex Transm Infect. 2012 Dec;88 Suppl 2(Suppl_2):i33-43. doi: 10.1136/sextrans-2012-050658. PMID: 23172344; PMCID: PMC3512431.
- Damtew B, Mengistie B, Alemayehu T. Survival and determinants of mortality in adult HIV/Aids patients initiating antiretroviral therapy in Somali Region, Eastern Ethiopia. Pan Afr Med J. 2015;22:1–8.
- Kee MK, Lee JH, Kim EJ, Lee J, Nam JG, Yoo BH, Kim SS. Improvement in survival among HIV-infected individuals in the Republic of Korea: need for an early HIV diagnosis. BMC Infect Dis. 2009 Aug 12;9:128. doi: 10.1186/1471-2334-9-128. PMID: 19671189; PMCID: PMC2738677.
- Pavlova-McCalla E, Trepka MJ, Ramirez G, Niyonsenga T. Socioeconomic Status and Survival of People with Human Immunodeficiency Virus Infection before and after the Introduction of Highly Active Antiretroviral Therapy: A Systematic Literature Review. J AIDS Clin Res. 2012 Jul 20;3(6):1000163. doi: 10.4172/2155-6113.1000163. PMID: 24575328; PMCID: PMC3933225.
- Mageda K, Leyna GH, Mmbaga EJ. High Initial HIV/AIDS-Related Mortality and -Its Predictors among Patients on Antiretroviral Therapy in the Kagera Region of Tanzania: A Five-Year Retrospective Cohort Study. AIDS Res Treat. 2012;2012:843598. doi: 10.1155/2012/843598. Epub 2012 Sep 2. PMID: 22973505; PMCID: PMC3437609.
- Sieleunou I, Souleymanou M, Schönenberger AM, Menten J, Boelaert M. Determinants of survival in AIDS patients on antiretroviral therapy in a rural centre in the Far-North Province, Cameroon. Trop Med Int Health. 2009 Jan;14(1):36-43. doi: 10.1111/j.1365-3156.2008.02183.x. Epub 2008 Nov 12. PMID: 19017309.
- Dias, Vera Junn, Eunsung Mouradian MM. Genetic alterations. NIH Public Access. Bone. 2008;23(1):1–7.
- Tadesse K, Haile F, Hiruy N. Predictors of mortality among patients enrolled on antiretroviral therapy in Aksum hospital, northern Ethiopia: a retrospective cohort study. PLoS One. 2014 Jan 31;9(1):e87392. doi: 10.1371/journal.pone.0087392. PMID: 24498093; PMCID: PMC3909114.
- Ayele W, Mulugeta A, Desta A, Rabito FA. Treatment outcomes and their determinants in HIV patients on Anti-retroviral Treatment Program in selected health facilities of Kembata and Hadiya zones , Southern Nations , Nationalities and Peoples Region , Ethiopia. BMC Public Health . 2015;1–13. http://dx.doi.org/10.1186/s12889-015-2176-5
- Wondimu W, Dube L, Kabeta T. Factors Affecting Survival Rates Among Adult TB/HIV Co-Infected Patients in Mizan Tepi University Teaching Hospital, South West Ethiopia. HIV AIDS (Auckl). 2020 Apr 23;12:157-164. doi: 10.2147/HIV.S242756. PMID: 32368156; PMCID: PMC7185339.
- Regional O, Forschen S. Determinants of Survival among Adults on Antiretroviral Therapy in Adama Hospital Medical. 2016.
- Tachbele E, Ameni G. Survival and predictors of mortality among human immunodeficiency virus patients on anti-retroviral treatment at Jinka Hospital, South Omo, Ethiopia: a six years retrospective cohort study. Epidemiol Health. 2016 Nov 6;38:e2016049. doi: 10.4178/epih.e2016049. PMID: 27820957; PMCID: PMC5309728.
- Joseph N, Sinha U, Tiwari N, Ghosh P, Sindhu P. Prognostic Factors of Mortality among Adult Patients on Antiretroviral Therapy in India: A Hospital Based Retrospective Cohort Study. Biomed Res Int. 2019 Jan 21;2019:1419604. doi: 10.1155/2019/1419604. PMID: 30805359; PMCID: PMC6363333.
- Zhang G, Gong Y, Wang Q, Deng L, Zhang S, Liao Q, Yu G, Wang K, Wang J, Ye S, Liu Z. Outcomes and factors associated with survival of patients with HIV/AIDS initiating antiretroviral treatment in Liangshan Prefecture, southwest of China: A retrospective cohort study from 2005 to 2013. Medicine (Baltimore). 2016 Jul;95(27):e3969. doi: 10.1097/MD.0000000000003969. PMID: 27399071; PMCID: PMC5058800.
- FMOH Ethiopia. National Consolidated Guidelines for Comprehensive Hiv Prevention , Care and. FMOH 2018;1–238. Available from: file:///C:/Users/Tere/Desktop/University of South Africa (17-2017)/Documents on Cervical Cancer/July 22,2017/All Litratures/National Comprehensive HIV Care Guideline 2018.pdf.
- Alemu AW, Sebastián MS. Determinants of survival in adult HIV patients on antiretroviral therapy in Oromiyaa, Ethiopia. Glob Health Action. 2010 Oct 29;3. doi: 10.3402/gha.v3i0.5398. PMID: 21042435; PMCID: PMC2967337.
- Beshir MT, Beyene AH, Tlaye KG, Demelew TM. Incidence and predictors of tuberculosis among HIV-positive children at Adama Referral Hospital and Medical College, Oromia, Ethiopia: a retrospective follow-up study. Epidemiol Health. 2019;41:e2019028. doi: 10.4178/epih.e2019028. Epub 2019 Jun 22. PMID: 31319659; PMCID: PMC6702120.
- Tchounga B, Ekouevi DK, Balestre E, Dabis F. Mortality and survival patterns of people living with HIV-2. Curr Opin HIV AIDS. 2016 Sep;11(5):537-544. doi: 10.1097/COH.0000000000000299. PMID: 27254747; PMCID: PMC5055442.
- Gupta A, Nadkarni G, Yang WT, Chandrasekhar A, Gupte N, Bisson GP, Hosseinipour M, Gummadi N. Early mortality in adults initiating antiretroviral therapy (ART) in low- and middle-income countries (LMIC): a systematic review and meta-analysis. PLoS One. 2011;6(12):e28691. doi: 10.1371/journal.pone.0028691. Epub 2011 Dec 29. PMID: 22220193; PMCID: PMC3248405.