More Information
Submitted: June 10, 2023 | Approved: June 20, 2023 | Published: June 21, 2023
How to cite this article: Tóth G. Celiac disease presenting as transient intussusception in two 3-year-olds. J Adv Pediatr Child Health. 2023; 6: 031-032.
DOI: 10.29328/journal.japch.1001057
Copyright License: © 2023 Tóth G. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Celiac disease presenting as transient intussusception in two 3-year-olds
Gergely Tóth*
Pediatric Department, Elisabeth Teaching Hospital Sopron, Semmelweis University, Hungary
*Address for Correspondence: Gergely Tóth, MD, PhD, Pediatric Department, Elisabeth Teaching Hospital Sopron, Semmelweis University, H-9400 Sopron, Győri Street 15, Hungary, Email: [email protected]
Although intussusception occurs in children and adults with celiac disease, it is a relatively uncommon symptom. Even more rare is the occurrence of intussusception as the presenting symptom of the disease. In the two cases we report here, transient intussusception, occurring at three years of age, was the first and only physical sign of celiac disease, and lead to a timely diagnosis by immunoserology and histology, followed by implementation of a gluten-free diet before sequelae such as significant anemia or Failure to Thrive (FTT) developed. In both cases, neither immunoserological nor physical signs of disease were present at the follow-up examination after 6 months on a gluten-free diet. In addition, genetic screening of the patients’ families revealed HLA-DQ2 positivity in two cases, leading to the additional diagnosis of celiac disease in the pregnant mother of one of the patients.
Celiac disease is an important differential diagnosis in cases of failure to thrive, weight loss, anemia, or chronic diarrhea in children. The scope of manifestations of the disease range from the so-called “silent” symptomless form to the most severe forms which can lead to Failure to Thrive (FTT). The number of individuals with “silent” celiac disease is thought to be far greater than the number who suffer from symptomatic forms, and even among those with symptoms mild disease is more common. There is a demonstrated genetic predisposition towards the development of some form of celiac disease.
Case 1
A 3-year-old boy was admitted to our inpatient department because of an upper respiratory tract infection (URTI). His history included multiple episodes of URTI associated with a low fever and gastroenteritis, with one Campylobacter jejuni-positive stool culture 6 months earlier. The patient appeared well-developed and well-nourished, and both his weight and height were within the normal range for his age [13.8 kg (25th percentile), 96 cm (50th percentile)]. He had no abdominal pain, or stool abnormalities, nor was anything abnormal, apart from the signs of URTI, found on physical examination. An abdominal ultrasound, performed as part of his basic clinical assessment, revealed an image typical of ileocolic intussusception, which spontaneously resolved during the examination (Figure 1). The patient showed no signs of discomfort during this process. His laboratory parameters showed no signs of inflammation (WBC: 7500 G/l, CRP: 1 mg/l, ESR: 5 mm/hr), anemia, or iron deficiency (Hgb: 120 g/l, Hct: 37%, Iron: 12 uM/l), and the examination of his stool for virus, bacteria, and parasites were negative. Immunoserological analysis revealed celiac disease-associated antibodies (anti-Gliadin: 2.6 U/ml; anti-tTG screen: 22.4 U/ml; anti-tTG IgA: 0.1 U/ml; anti-tTG IgG: 145.4 U/ml; EMA IgA: negative; EMA IgG: positive). On the basis of these findings, we performed an upper GI endoscopy, and a histological examination of a biopsy taken from the small intestine found partial villous atrophy (PVA, Marsh 3/a). Genetic analysis revealed that the patient was HLA-DQ2 positive. We made the diagnosis of gluten-sensitive enteropathy and recommended a gluten-free diet. At the 6-month follow-up examination, the patient was symptom-free, and celiac-associated antibodies were negative. We screened the family members of the patient for celiac disease and found that his mother (who happened to be pregnant at the time) had positive immunoserology results and flat mucosa (Marsh 3/b) in the biopsy taken from her small intestine.
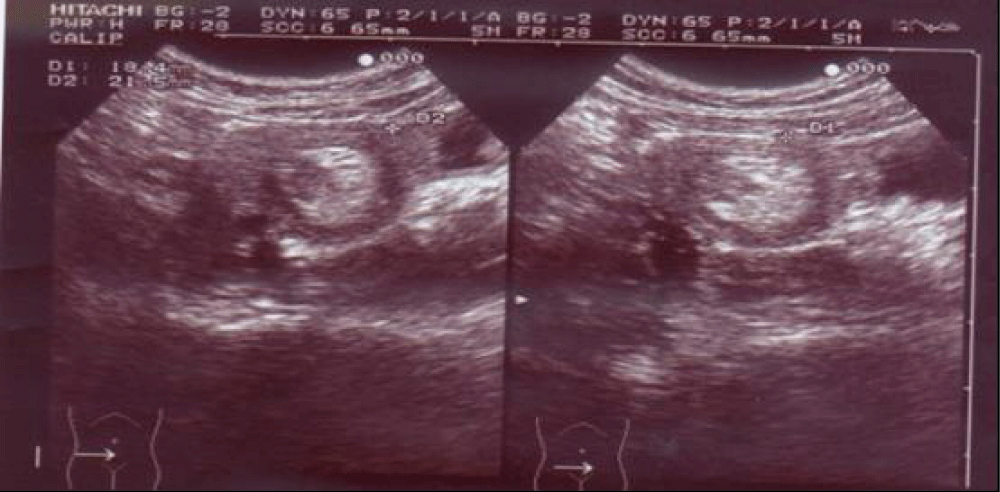
Figure 1: Abdominal US: On the right side of the umbilicus, a 23 mm diameter pathological target sign and approximately a dozen 10 mm lymph nodes are visible. The intussusceptum resolved in a matter of minutes. Radiological opinion: US indicative of intussusception, but no typical clinical signs present.
Case 2
A 3-year-old girl was referred to our clinic with abdominal pain which recurred weekly. Her history did not reveal any potentially related events or illnesses, and she was developing well [weight 15 kg (50th percentile), length 93 cm (25th percentile)] with a good appetite. The patient had no stool abnormalities, nor was any pathology revealed on physical examination. An abdominal ultrasound examination revealed an ileocolic intussusception, which spontaneously resolved during the examination and caused the patient no visible discomfort (Figure 2). Laboratory examinations revealed no sign of acute inflammation (WBC: 6500 G/l; CRP: 3 mg/l; ESR: 7 mm/hour), but mild iron-deficiency anemia (Hgb: 110 g/l; Hct: 34%; Iron: 4.5 mM/l) and slightly elevated aspartate transaminase levels (GOT/AST 57 U/l) were present. The patient’s stool was negative for viral, bacterial, and parasitic pathogens. Immunoserological examination revealed celiac-related antibodies (anti-Gliadin: >100,0 U/ml; anti-tTG Screen: >100,0 U/ml; anti-tTG IgA: >100,0 U/ml; anti-tTG IgG: 66,7 U/ml; EMA IgA: positive; EMA IgG: positive). A biopsy of the small intestine revealed partial villous atrophy (PVA, Marsh 3/a), and a genetic analysis found that the patient was HLA-DQ2 positive. We considered the patient’s recurrent abdominal pain to be caused by recurrent intussusception related to celiac disease and, and prescribed a gluten-free diet. At the 6-month follow-up visit the patient was symptom-free, there was no sign of intussusception on abdominal ultrasound, and the immunoserological analysis was negative for celiac-related antibodies. Upon screening of the family, the patient’s father was found to be HLA-DQ2 positive but had no signs of celiac disease.
Figure 2: Abdominal US: In the ileo-coecal region, a 2 cm diameter target sign is visible. Radiological opinion: image is typical of intussusception, but considering the clinical condition of the patient this is very unlikely.
These two cases of intussusception as the presenting feature of celiac disease in young children add to the few reports of such cases in the literature, and reinforce the need to consider celiac disease in cases of intussusception, even if the typical symptoms of the disease (diarrhea, weight loss, anemia, failure to thrive) are not present [1]. Particularly notable in the two cases reported here is that the children were well within the normal ranges for weight and height, only one of the two had mild anemia and elevation of liver enzymes, and neither showed evidence of Failure to Thrive (FTT), which was the reason for examination in several other cases reported in the literature. These cases also demonstrate the broad spectrum of severity in celiac disease, from genetic predisposition to symptomatic disease, and the usefulness and importance of screening the immediate family members once the diagnosis is made.
HLA types DQ2 and DQ8 are useful negative predictors of celiac disease, with studies showing that if the patient is negative for both, there is almost 100% certainty that she is not suffering from celiac disease.
Once intussusception was observed at this atypical age, immunoserology can and should be used as a simple method to exclude celiac disease [2]. If the serology is positive, then the definitive diagnosis can be established by biopsy of the small intestine. Furthermore, establishing whether or not the patient is HLA-DQ2 or –DQ8 positive can be useful for reinforcing or refuting the diagnosis, as those individuals not possessing these HLA types are almost 100% certain not to have celiac disease.
In summary, our two cases show that toddlers or children with mild, chronic abdominal pain without diarrhea and failure to thrive have to be examined properly. If the infection can be excluded and the abdominal US reveals intussusception with a good clinical condition of the patient, celiac disease has to be considered as a cause of bowel hypermotility manifesting in transient intussusception.
Celiac disease appears to be associated with a modestly increased risk of intussusception, although most of these cases remain asymptomatic. Debate still continues as to whether all patients of intussusception should be screened for celiac disease [3].
- Goyal P, Nohria S, Singh Grewal C, Sehgal R, Goyal O. Celiac disease and intussusception - a rare but important association. Acta Gastroenterol Belg. 2022 Jan-Mar;85(1):111-112. doi: 10.51821/85.1.7959. PMID: 35305004.
- Brown NK, Guandalini S, Semrad C, Kupfer SS. A Clinician's Guide to Celiac Disease HLA Genetics. Am J Gastroenterol. 2019 Oct;114(10):1587-1592. doi: 10.14309/ajg.0000000000000310. PMID: 31274511.
- Borkar VV, Poddar U, Thakral A, Agarwal J, Srivastava A, Yachha SK, Kumar S. Intussusception in celiac disease: Is it a common feature in children? J Gastroenterol Hepatol. 2018 Feb;33(2):380-384. doi: 10.1111/jgh.13865. PMID: 28688105.